Obstructive Sleep Apnea (OSA) is a disorder that, while often disregarded, has a major effect on the quality of life and longevity of millions of people worldwide. Imagine waking up after a night of “peaceful sleep,” only to find your body tired and your mind foggy , as if it had never actually rested. Obstructive Sleep Apnea is the cause of this disorder, which quietly disrupts sleep and puts people at risk for a variety of significant health problems, including cardiovascular disease, stroke, and death. Are we living with this threat without even knowing it? Let’s explore OSA with CLM Sleep in the article below.
Obstructive sleep apnea overview
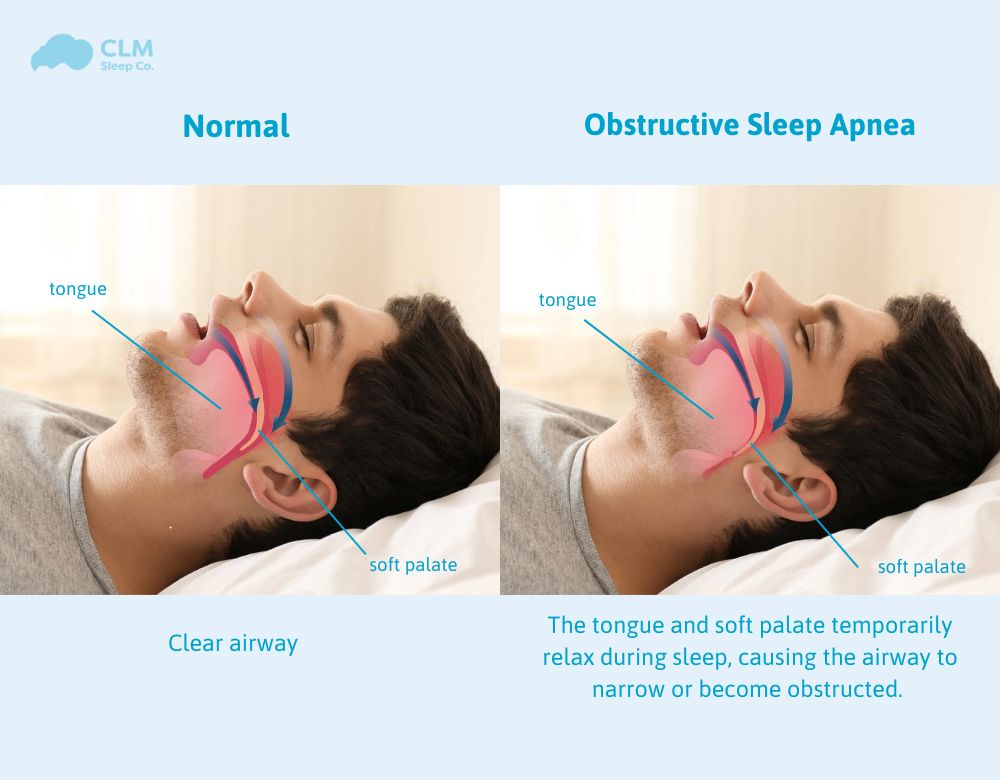
Obstructive Sleep Apnoea is a common yet serious sleep disorder characterised by repeated interruptions in breathing during sleep. This occurs when the muscles that support the soft tissues in your throat, such as your tongue and soft palate, temporarily relax. When these muscles relax, your airway is narrowed or closed, and breathing is momentarily cut off.
These episodes of obstruction may happen many times – even hundreds of times – overnight, with each episode lasting from seconds to minutes. Some people realise that they don’t breathe very well at night but may be unaware that this is a medical issue that is causing them harm. Fortunately, overnight tests are readily available and a variety of treatments exists.
How Obstructive Sleep Apnea Differs from Central Sleep Apnea?
Obstructive sleep apnea results from a physical blockage in the airway. Central sleep apnea occurs when the brain fails to transmit the necessary signals to the muscles that control breathing. There is no physical obstruction in central sleep apnea. It’s simply that the body stops trying to breathe for a short period of time. Both disorders impair sleep, but their causes are fundamentally different and necessitating distinct treatment approaches.
See more: 03 Types Of Sleep Apnea OSA, CSA, CompSAS: Symptoms, Treatment
Symptoms and Causes
Symptoms of Obstructive Sleep Apnea
The most common symptom of obstructive sleep apnoea is loud, chronic snoring, often followed by gasping or choking sounds as breathing resumes. However, not all people who snore have sleep apnoea. Other symptoms include excessive daytime sleepiness, morning headaches, difficulty concentrating, and irritability. Sleep apnoea can affect people of all ages and body types, though it is more prevalent in middle-aged, overweight individuals.
The table below lists the symptoms commonly seen in obstructive sleep apnea:
| Symptoms | Features |
| Symptoms during sleep | |
| Loud snoring | Snoring is loud, frequent, and may vary in volume |
| Panic breathing | Short pauses in breathing during sleep, which may be recognized by jerks or noises. |
| Irregular breathing | Breathing may stop and start again suddenly |
| Difficulty sleeping | Having trouble staying asleep and waking up several times during the night. |
| Feeling breathless | Feeling short of breath or like you are choking while sleeping. |
| Symptoms when waking up | |
| Dry breathing | Your mouth or throat may feel dry after sleeping |
| Feeling tired | Feeling tired or lethargic even after getting enough sleep |
| Morning headaches | Headaches upon waking, often due to lack of oxygen during the night. |
| Dry mouth | Your mouth may feel dry when you wake up, especially if you breathe through your mouth while sleeping. |
| Daytime symptoms | |
| Daytime fatigue | Feeling sleepy, tired, or lacking energy throughout the day. |
| Difficulty concentrating | Difficulty concentrating, decreased ability to remember or process information. |
| Mood changes | Feeling more irritable, anxious, or depressed than usual. |
| Reduced work performance: | Decreased ability to work or difficulty performing daily tasks. |
| Other symptoms | |
| Sleep disturbances | You may experience problems such as sleepwalking, light sleep, or nightmares. |
| Sexual problems | Decreased sex drive |
When to see a doctor
It’s crucial to consult a doctor if you notice loud snoring that disrupts your sleep, if you experience pauses in breathing during the night, or if you suffer from severe daytime fatigue that affects your daily routine. These signs could be indicative of obstructive sleep apnea or another sleep disorder that needs professional evaluation and treatment.
See more: Identifying Sleep Apnea Symptoms: Are You at Risk?
Causes
Obstructive sleep apnea occurs when the muscles in the throat relax excessively during sleep, leading to a narrowed or blocked airway. This can be due to factors like excess weight, big tonsils, or a narrowed airway. And other contributing factors include smoking, alcohol use, nasal congestion, or a family history of sleep apnea. Below are some reasons that can cause upper airway obstruction during sleep, leading to sleep apnea:
Relaxation of Throat Muscles
During sleep, the muscles at the back of the throat relax too much, causing the airway to collapse or become blocked. This relaxation can obstruct airflow, leading to pauses in breathing.
Excess weight
Obesity is a major risk factor, as excess fat can accumulate around the neck and throat, contributing to airway obstruction. Increased fat deposits can put pressure on the airway, making it more likely to collapse.
Big Tonsils and Adenoids
In both children and adults, enlarged tonsils and adenoids can obstruct the airway. These structures can obstruct the throat, especially in children, who are more susceptible to this issue.
Structural Issues
Issues with the structure of the airway, such as a thick neck, a large tongue, or a deviated septum, can narrow the airway, making it more prone to obstruction.
Nasal Congestion
Chronic nasal congestion or conditions like sinusitis can lead to difficulties in breathing through the nose. This can force individuals to breathe through their mouth, which may increase the risk of airway obstruction.
Genetics
A family history of OSA or related conditions can increase the risk of developing the disorder.
Mechanism: Genetic predisposition may influence the structure of the airway or other contributing factors.
Age
The risk of OSA increases with age. Aging can lead to a decrease in muscle tone and elasticity in the throat, making the airway more prone to collapse.
Gender
Men are more likely to develop OSA than women. Hormonal and anatomical differences can contribute to a higher risk in men.
Contributing Factors
Alcohol: A stimulant that weakens the normal functioning of the throat muscles, which can increase the likelihood of airway collapse, worsening OSA.
Smoking: Smoking causes irritation and inflammation of the airways, leading to swelling and increased mucus production, which results in airway obstruction.
Medications: Some muscle relaxants or sedatives can exacerbate the condition of airway obstruction.
Risk Factors for Obstructive Sleep Apnea
Anatomic Factors
- Excess Weight
- Enlarged Tonsils and Adenoids
- Narrow Airway
- Structural Abnormalities
Nonanatomic Risk Factors
- Smoking
- Alcohol Use
- Nasal Congestion
- Family History
Additional Factors
- Age
- Gender
Associated Medical Disorders
Hypertension: High blood pressure is commonly associated with OSA.
Type 2 Diabetes: People with OSA are at a higher risk for developing insulin resistance and type 2 diabetes.
Heart Disease: OSA can contribute to cardiovascular problems, including heart failure and arrhythmias.
Stroke: There is an increased risk of stroke in individuals with untreated OSA.
How obstructive sleep apnea depends on age and gender? (male, female)
People of any age can develop OSA, but older adults are at a higher risk because the muscles in the throat weaken and the airways are more prone to collapse.In addition, OSA also occurs in children, often related to big tonsils and adenoids or some other congenital airway conditions.
Men are generally at a higher risk of developing OSA compared to women. Partly due to anatomical differences such as a thicker neck or a greater distribution of fat in the neck area.
Complications
Untreated sleep apnoea can lead to severe health complications, including hypertension, heart disease, stroke, and diabetes. It can also increase the risk of motor vehicle and workplace accidents due to sleep deprivation. Moreover, poor sleep quality can impact mental health, contributing to depression and anxiety. Below are the common complications of patients with obstructive sleep apnea.
Cardiovascular Problems
Hypertension (High Blood Pressure): OSA can cause sudden drops in blood oxygen levels during sleep, which increases blood pressure and strains the cardiovascular system. This can lead to chronic high blood pressure (hypertension).
Heart Disease: OSA increases the risk of heart attacks, heart failure, and other cardiovascular diseases due to repeated episodes of low oxygen levels and the resulting stress on the heart.
Arrhythmias: OSA can lead to irregular heartbeats, such as atrial fibrillation. These arrhythmias can be triggered by the frequent drops in oxygen levels and the increased stress on the heart.
Stroke
People with untreated OSA have a higher risk of stroke, potentially due to the impact of repeated oxygen deprivation on brain function and blood vessels.
Type 2 Diabetes
OSA is associated with insulin resistance, which can increase the risk of developing type 2 diabetes. The repeated awakenings and poor sleep quality associated with OSA may also impact glucose metabolism.
Daytime Fatigue and Cognitive Impairment
Excessive Daytime Sleepiness: OSA often leads to severe daytime sleepiness, reducing alertness and increasing the risk of accidents, especially when driving or operating machinery.
Cognitive Impairment: Poor sleep quality can affect concentration, memory, and decision-making skills, leading to decreased work performance and reduced quality of life.
Mood Disorders: OSA is linked to mood disorders such as depression, anxiety, and irritability due to disrupted sleep and fatigue.
Metabolic Syndrome
OSA is associated with metabolic syndrome, which includes a combination of conditions such as high blood pressure, high cholesterol, increased waist circumference, and high blood sugar levels. These conditions increase the risk of heart disease, stroke, and diabetes.
Liver Problems
People with OSA are more likely to have abnormal liver function tests and evidence of nonalcoholic fatty liver disease (NAFLD), a condition in which fat builds up in the liver cells.
Complications with Surgery and Medications:
OSA can cause complications with surgery, as individuals with OSA may be more prone to airway obstruction while under anesthesia or sedation. Additionally, they may be more sensitive to sedative medications, which can worsen breathing issues.
Reduced Quality of Life
The combined effects of OSA, such as excessive fatigue, cognitive impairment, mood disturbances, and increased health risks, can significantly reduce the overall quality of life and well-being.
Increased Risk of Accidents
Due to excessive daytime sleepiness and reduced alertness, individuals with untreated OSA are at higher risk for motor vehicle accidents, workplace accidents, and falls.
Diagnosis and Treatment
Diagnosis and Tests
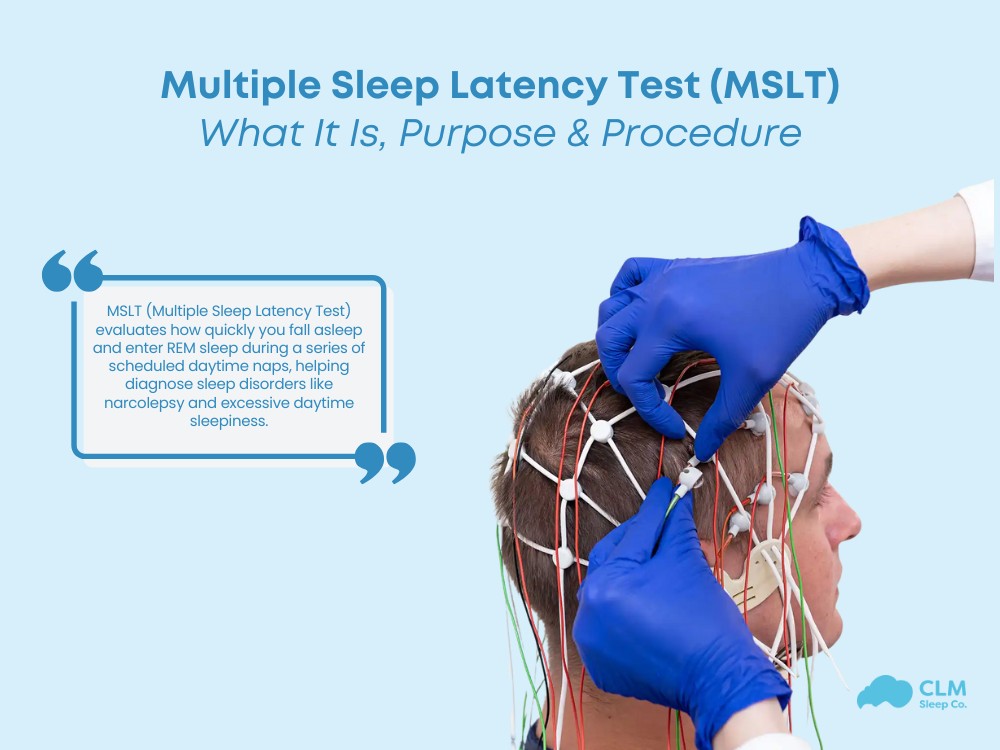
Usually, diagnosis involves an overnight sleep study called a polysomnogram, which monitors breathing patterns, heart rate, and oxygen levels during sleep. This may be conducted in a sleep laboratory or home, depending on your needs and doctor’s recommendations.
How to obstructive sleep apnea test at home?
Management and Treatment
The gold standard treatment for OSA is the continuous positive airway pressure (CPAP) machine, which keeps the airway open by providing a steady stream of air through a mask. For some people, an oral sleep appliance (Mandibular Advancement Splint) fitted by a specialist dentist which holds the jaw forward during the night to keep the airway open may be a suitable treatment. For milder cases, lifestyle changes such as weight loss, avoiding alcohol, and sleeping on one’s side may help. There are also several surgical options available when all other treatment options have been exhausted and have not helped.
Departments and Specialties
Departments that treat obstructive sleep apnea
Sleep medicine
Sleep medicine is the main field that assesses and manages sleep disorders, including OSA. Experts in this department conduct research on sleep and develop personalized treatment plans.
Ear, Nose, and Throat (ENT)
Ear, Nose, and Throat specialists (otolaryngologists) often treat patients with OSA due to anatomical issues such as enlarged tonsils and adenoids or nasal obstruction.
Pulmonologists
Pulmonologists specialize in treating lung and respiratory problems. They can help manage OSA, especially when it is associated with other respiratory disorders.
Cardiovascular system
In cases where OSA affects cardiovascular health, cardiologists may be involved in patient care to manage conditions such as hypertension or arrhythmias.
Endocrine
Endocrinologists can participate in the treatment of patients with OSA related to metabolic issues such as obesity or type 2 diabetes.
Obstructive sleep apnea treatment specialist
Sleep specialists: Doctors trained specifically to diagnose and manage sleep disorders, including OSA, are often certified in sleep medicine.
Ear, nose, and throat specialist (ENT specialist): The doctor can perform surgeries such as tonsillectomy, adenoidectomy, or other procedures to alleviate airway obstruction.
Pulmonologist: A respiratory specialist who helps manage OSA, especially when this condition is accompanied by other lung diseases.
Dentists or orthodontists: Specialists who create oral devices to help keep the airway open during sleep.
Surgeons: Such as maxillofacial surgeons, who may perform more complex surgeries (e.g., jaw advancement surgery) to correct structural problems contributing to obstructive sleep apnea (OSA).
Treating doctor
Primary care physicians are often the first to evaluate symptoms and refer patients to specialists for diagnosis and treatment.
Sleep Medicine Physicians are specialists who diagnose and provide comprehensive treatment programs for OSA.
Respiratory Therapists: They are frequently involved in maintaining Continuous Positive Airway Pressure (CPAP) therapy and educating patients on its use.
Prevention
Maintaining a healthy weight: Losing excess weight, especially around the neck area, can reduce the risk of airway obstruction.
Sleeping position: Sleeping on your side instead of on your back can help prevent airway collapse.
Avoid alcohol and sedatives: Limiting the use of alcohol and sedatives, especially before bedtime, can reduce the relaxation of the muscles in the throat.
Regular exercise: Engaging in physical activities regularly can help improve overall health, reduce the risk of obesity, and enhance sleep quality.
Quitting smoking: Quitting smoking can reduce inflammation and swelling in the upper respiratory tract, helping to lower the risk of developing OSA.
Outlook / Prognosis
Short-Term Outlook: With a proper diagnosis and appropriate treatment, such as CPAP therapy, oral or dental appliances, or surgery. Most individuals experience significant improvements in their symptoms and quality of life. Correctly managing OSA in the short term can alleviate daytime sleepiness, improve concentration, and enhance mood, leading to better daily functioning.
Long-Term Prognosis: Effectively managing OSA can reduce the risk of severe complications, including cardiovascular disease, stroke, and diabetes. When OSA is left untreated, however, it can lead to worsening health outcomes, a lower quality of life, and an increased risk of mortality. Efficient treatment is crucial in mitigating these risks and ensuring long-term health benefits.
Continued Monitoring: Regular follow-up visits with healthcare providers are essential to adjust treatment as needed and monitor for any new or worsening symptoms. Ongoing monitoring helps ensure that the treatment remains effective and addresses any changes in the patient’s condition promptly, maintaining optimal management of OSA over time.
Living with obstructive sleep apnea
Adherence to Treatment: Consistent use of prescribed treatments, like CPAP, oral appliances, or lifestyle changes, is crucial to managing symptoms effectively.
Healthy Sleep Hygiene: Establishing a regular sleep schedule, creating a comfortable sleep environment, and avoiding stimulants before bedtime can help improve sleep quality.
Monitoring for Complications: Regular check-ups to monitor for related health conditions, such as hypertension, diabetes, or heart disease, are important.
Support and Education: Joining a support group or working with a healthcare team to understand OSA and its management can provide encouragement and help maintain a positive outlook.
Communication with Healthcare Providers: Maintain open communication with healthcare providers about symptoms, treatment side effects, or any difficulties helps in optimizing management strategies.
Obstructive sleep apnea CLM Sleep Co.
At CLM Sleep, we take an individualized and holistic approach to diagnosing issues affecting sleep and overall health. Our team of specialists in sleep and respiratory medicine collaborates with leading sleep scientists to provide high-quality diagnostic and treatment services for individuals suffering from sleep apnea. Our carefully trained and selected consultants adhere to the highest standards of the industry. With patient-centered care services and a strategy to update the latest treatment methods. CLM Sleep provides patients with the most effective and suitable treatment regimen. Includes CPAP therapy, positional therapy, oral appliances, dietary and weight management, and sleep training, along with many other options.
Conclusion of the article
Sleep apnoea is a manageable condition, but it requires timely diagnosis and treatment to prevent long-term health complications. If you or someone you know exhibits symptoms of sleep apnoea, speak to your GP or come into CLM Sleep Co. to speak to our friendly staff and we will guide you through the next steps to getting diagnosed and treated promptly.