Sleep apnea is a very serious sleep disorder related to the occurrence of short periods of breathing cessation during sleep, which can last from several seconds to a few minutes. Based on the number of apneas and hypopneas, the Apnea-Hypopnea Index (AHI) has been developed and used to determine the presence and severity of sleep apnea. AHI divides sleep apnea into three levels: mild, moderate, and severe. Determining the correct level of the condition you are experiencing can help you better manage sleep apnea and receive more accurate treatment. To know more details about AHI sleep apnea, read the article below from CLM Sleep.
What is AHI in sleep apnea?
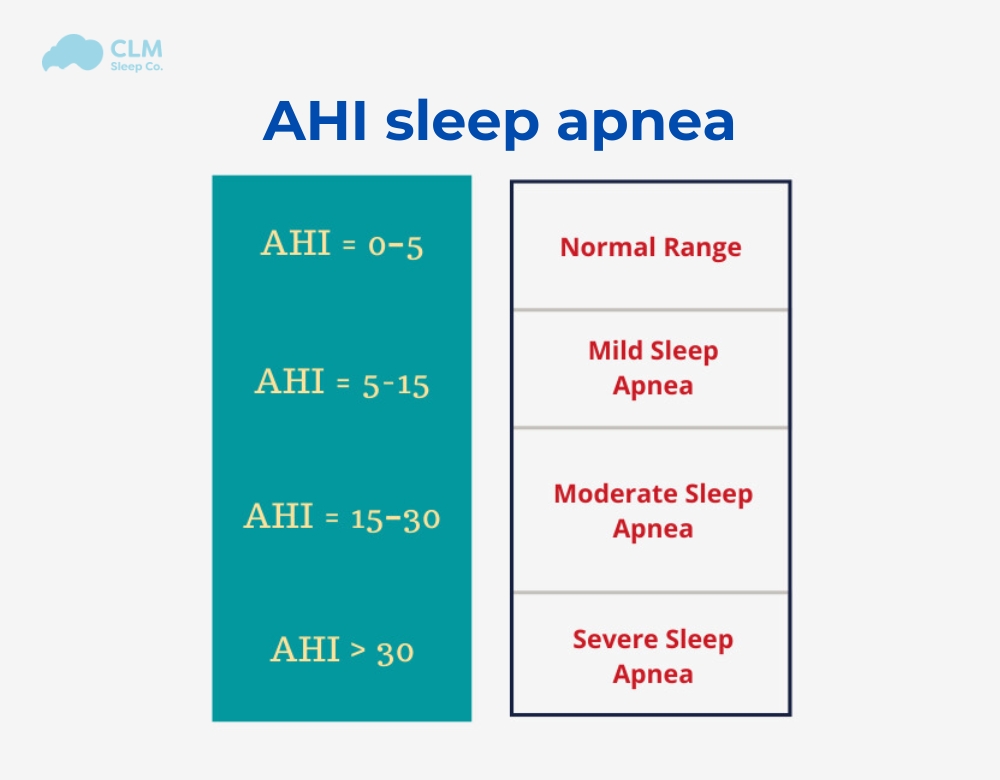
AHI (apnea-hypopnea index) is the average number of apnea and hypopnea episodes occurring per hour of sleep. Put simply, your AHI shows how many times your breathing stops or gets weaker every hour while you’re asleep, which helps sleep specialists diagnose sleep apnea and assess its severity. Therefore, this index is often referred to as the AHI sleep apnea. The higher the AHI, the more severe the sleep apnea.If your AHI < 5, your breathing is considered normal. Sleep apnea is diagnosed when your AHI ≥ 5. The severity of sleep apnea in adults is determined as follows: Mild sleep apnea: 5 ≤ AHI < 15; Moderate sleep apnea: 15 ≤ AHI < 30; Severe sleep apnea: AHI ≥ 30.
AHI pediatric
In children, the AHI index is also used to assess the severity of sleep apnea by counting the number of apneas (breath pauses) and hypopneas (shallow breaths) per hour of sleep. However, the criteria for determining severity differ from those used for adults.
- Normal: < 1 episode/hour
- Mild Sleep Apnea: 1–5 episodes/hour
- Moderate Sleep Apnea: 5–10 episodes/hour
- Severe Sleep Apnea: > 10 episodes/hour
See more: Sleep Apnea in Children
Calculating AHI
AHI is calculated by dividing the number of times apneas and hypopneas occur by the total hours of sleep
AHI= (Apneas+Hypopneas)/Hours of sleep AHI
For instance, it would imply that with 40 episodes over some time of 8 hours, an individual’s AHI would be 5, therefore standing for mild sleep apnea. The success in treatments, such as CPAP therapy, is normally monitored based on the record of the AHI sleep apnea over time. AHI index as a measure of sleep apnea severity

Classification of sleep apnea severity through the AHI index
AHI is the standard method for determining the severity of sleep apnea. In addition to analyzing the symptoms of sleep apnea, AHI will help you determine the severity of sleep apnea quickly, effectively, and accurately. The higher the AHI, the more severe the sleep apnea. CLM Sleep will help you easily differentiate between the different levels of sleep apnea.
Mild Sleep Apnea
Mild sleep apnea is characterized by an AHI between 5 and 14. In this category, the person experiences 5 to below 15 breathing interruptions per hour during sleep. Though all symptoms of mild sleep apnea may not be serious and significant during the daytime, common results could include mild tiredness, drowsiness, and/or slight lapses in concentration. This early stage can often be improved, and further progression may be prevented through simple changes in lifestyle or mild CPAP therapy.
Moderate Sleep Apnea
An AHI of 15 to below 30 defines moderate sleep apnea. In such cases, the person experiences 15 to 29 events of apnea or hypopnea per hour, which results in more recognizable sleep disturbances. Other symptoms may include daytime sleepiness, headaches, and difficulty concentrating. The risk of hypertension and cardiovascular issues at this level begins to rise, thus rendering treatment an important consideration.
Severe Sleep Apnea
Severe sleep apnea is when the AHI is 30 or higher. In this case, a person with severe sleep apnea stops breathing or pauses more than 30 times per hour of sleep. As a result, such sleepers would be highly affected and their quality of sleep would be severely affected. Individuals experiencing severe sleep apnea bear a high risk for the complications of serious health issues, including heart disease, stroke, diabetes, and impaired cognitive function. Therefore, immediate and aggressive treatments, such as CPAP therapy or even surgical alternatives, are usually necessary to manage the condition effectively.
| AHI Severity Level | AHI Range (Events per Hour) | Description |
| Normal | Less than 5 | Breathing events are within normal range, indicating no clinically significant sleep apnea |
| Mild sleep apnea | 5 to 14 | Mild sleep apnea is present. Though not severe, it’s the gateway to understanding sleep health better. |
| Moderate sleep apnea | 15 to 29 | Moderate sleep apnea has encroached; a nudge to take action. |
| Severe sleep apnea | 30 or more | Severe sleep apnea is at play, demanding urgent intervention. |
Health Implications of AHI
AHI is one of the most critical parameters in determining sleep apnea and its consequences for an individual’s health and well-being. Therefore, the higher the AHI, the greater are the health consequences. Given below are some of the basic points for the health implications concerning AHI levels:
Cardiovascular Issues
People with higher AHI sleep apnea scores are more likely to develop cardiovascular-related disorders such as hypertension, heart attack, and stroke. According to a study published in Sleep Medicine, every 10-point increase in AHI score is associated with a 9% higher risk of developing cardiovascular disease. It could be because the frequent disruption in breathing leads to fluctuating oxygen levels that stress out the cardiovascular systems. Over time this can lead to chronic conditions that heavily impact the health of a person’s heart.
Metabolic Disorders
Sleep apnea is related to metabolic syndrome, which includes conditions such as, but not limited to, obesity, insulin resistance, and type 2 diabetes. This intermittent hypoxia may disturb metabolic processes, further enhancing the susceptibility to such disorders and complicating weight management and blood sugar regulation.
Daytime Fatigue and Cognitive Impairment
Higher levels of AHI are related to higher levels of daytime sleepiness and cognitive impairment. The continuous disturbance in sleep may promote a condition whereby restful stages of sleep are never achieved, thus creating symptoms such as fatigue, decreased alertness, and difficulties in memory and concentration. Consequently, this may lead to impacts on daily functioning and quality of life, increased risk for accidents, and decreased productivity.
Mental Health Effects
Anxiety and depression are among the mental disorders that may be linked to sleep apnea. The fatigue and sleep disruption may lead to mood changes and irritability; overall, this contributes to a decline in mental well-being. Treatment of sleep apnea may improve mood and emotional health.
Increased Risk of Complications During Surgery
Individuals with moderate to severe sleep apnea carry increased health risks because of possible anesthesia and respiratory complications associated with the condition. Healthcare professionals need to know if a patient has an AHI before surgery to mitigate risks.

How AHI is Measured
The Apnea-Hypopnea Index (AHI) is assessed through various methods, each with its advantages and levels of detail. Here are the primary approaches:
In lab Polysomnography
Sleep study – Polysomnography (PSG) is the gold standard for measuring AHI sleep apnea. Conducted in a sleep lab, this comprehensive sleep study monitors multiple physiological parameters, including:
- Electroencephalogram (EEG): Records brain activity to identify sleep stages.
- Oximetry: Measures oxygen levels in the blood.
- Airflow Sensors: Detects breathing patterns and interruptions.
- Electrocardiogram (ECG): Monitors heart rate.
- Muscle Activity: Assesses movement during sleep.
The extensive data collected allows for precise identification of apneas and hypopneas, which are crucial for calculating the AHI accurately.
The extensive data collected from in-lab Polysomnography allows for precise identification of apneas and hypopneas, which are crucial for accurately calculating the AHI.
Home Sleep Apnea Test (HSAT)
Home Sleep Apnea Testing (HSAT) is a convenient option for diagnosing sleep apnea outside a clinical setting. It typically involves:
- Simplified Monitoring: HSAT devices usually track fewer parameters, such as airflow, oxygen saturation, and heart rate.
- User-Friendly Equipment: Patients can set up the equipment at home, making it more accessible.
While HSAT provides valuable information, it may not capture the full complexity of sleep disorders compared to PSG, but it is effective for diagnosing obstructive sleep apnea in many cases.
Sleep Tracking Devices
Wearable sleep-tracking devices, such as smartwatches and fitness bands, are increasingly popular for monitoring sleep patterns. These devices may offer:
- Basic Data: They typically track sleep duration, movement, and heart rate.
- User Insights: While not specifically designed to measure AHI, some devices provide insights into sleep quality and potential apnea events.
However, the accuracy and reliability of consumer-grade sleep trackers for diagnosing sleep apnea are limited, and they should not replace professional evaluations.
Clinical Symptom Analysis
In addition to physiological measurements, clinical symptom analysis plays a crucial role in diagnosing sleep apnea. Healthcare providers consider:
- Patient History: Information about snoring, gasping, or choking during sleep.
- Daytime Symptoms: Fatigue, excessive sleepiness, and cognitive impairments.

Treatment for Sleep Apnea
Sleep apnea treatment varies based on the severity of the condition and individual patient needs. Here are the primary treatment options:
Lifestyle Changes
- Weight Loss: Reducing weight can alleviate symptoms of obstructive sleep apnea.
- Positional Therapy: Sleeping on the side helps keep the airway open.
- Avoiding Alcohol and Sedatives: These relax throat muscles and worsen apnea.
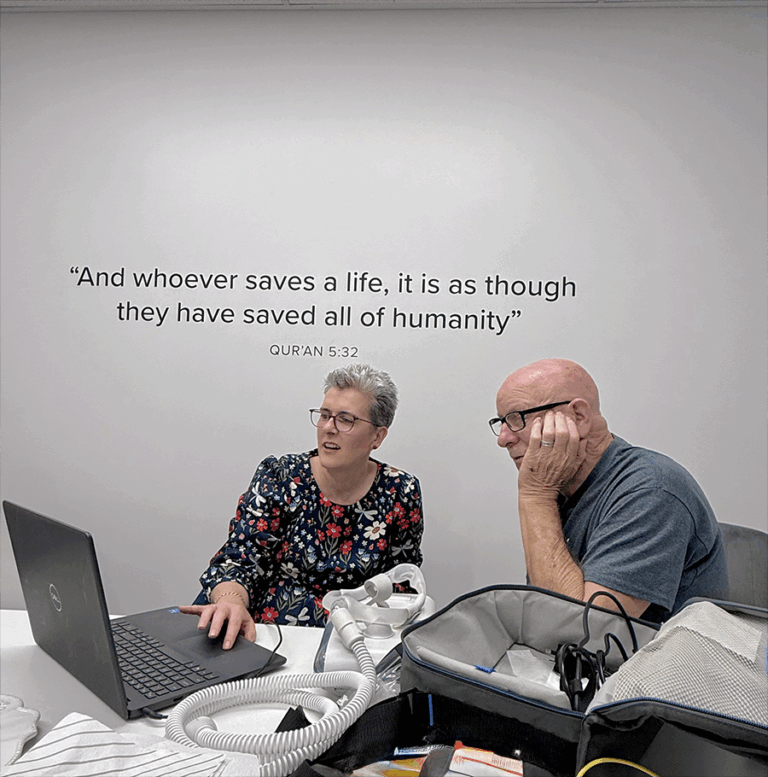
CPAP Therapy
- AHI in sleep apnea with CPAP Machine: Delivers air through a mask to keep the airway open during sleep.
- Adjustment: It may take time to get used to, but adherence is key.
Oral Appliances: Dental devices reposition the jaw and tongue to keep the airway open, especially for mild to moderate cases.
Surgery: Procedures like UPPP or jaw advancement address anatomical causes.
Supplemental Oxygen: Oxygen may be prescribed for severe cases to maintain proper levels during sleep.
In conclusion, understanding AHI sleep apnea is vital for diagnosing and managing sleep apnea effectively. For more information on sleep apnea treatments and helpful products, visit the website of CMLSleep. We offer comprehensive diagnostic and treatment services for sleep apnea, helping you restore sleep quality and enhance your health.
Start your journey to better sleep today!
Hotline: 1300 256 753
Head Office: CLM – Sleep Study Kent Town, Adelaide
Reference
- Jui-Kun Chiang, Yen-Chang Linet et al. Correlation between snoring sounds and obstructive sleep apnea in adults: a meta-regression analysis. Sleep Science. 2022 Oct-Dec;15(4):463–470. doi: 10.5935/1984-0063.20220068. PMCID: PMC9670768 PMID: 36419807.
- Hudgel DW. Sleep Apnea Severity Classification – Revisited. Sleep. 2016 May 1;39(5):1165–1166. doi:10.5665/sleep.5776. PMCID: PMC4835315
- Asghari A, Mohammadi F. Is Apnea‑Hypopnea Index a proper measure for Obstructive Sleep Apnea severity? Med J Islam Repub Iran. 2013 Aug;27(3):161–162. PMID: 24791128; PMCID: PMC3917481.
- Gouthro K, Slowik JM. Pediatric Obstructive Sleep Apnea. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan 1. PMID: 32491542; Bookshelf ID: NBK557610.
- Zhang X, et al. Association between obstructive sleep apnoea syndrome and the risk of cardiovascular diseases: an updated systematic review and dose‑response meta‑analysis. Sleep Med. 2020 Jul;71:39–46. DOI :10.1016/j.sleep.2020.03.011. PMID: 32485597