The sleep apnea test is used to monitor sleep while diagnosing sleep apnea, an intensely dangerous sleep disorder wherein respiration is repeatedly interrupted during sleep. The test keeps track of important functions like heart rate, breathing, and oxygen levels. Early detection facilitated by this test can keep complications like heart disease, stroke, and daytime fatigue at bay. Explore more information on how the sleep apnea test is performed and why this test is important for healthy sleep via the below article from CLM Sleep.
Types of Sleep Apnea Tests
The sleep apnea test can be classified into two main types, each serving different diagnostic purposes:
In-lab Polysomnography (PSG)
An overnight polysomnography diagnostic test for sleep-related breathing disorders. And other conditions is available at first inpatient service and includes narcolepsy and other forms of sleep motor restlessness. Patients are connected to different monitoring devices. This allows surveillance of changes in physiological variables like brain activity, eye movements, heart and lung function, and blood oxygen levels during sleep. It gives meaningful insight into sleep cycles and is probably preferable to the former in all but mild cases of suspected sleep apnea or when other sleep disorders are suspected.

Home Sleep Apnea Test (HSAT)
Home Sleep Apnea Testing (HSAT or HST) is a simple, minimally invasive, and low-cost overnight test that can be done from the convenience of your own home. Portable devices are used for HSAT that monitor some important parameters like airflow, effort of breathing, and oxygen saturation when a person is asleep. It is appropriate for home sleep apnea testing in people who are at moderate to high risk for developing sleep apnea. However, it is not a replacement for the gold standard test called Polysomnography (PSG) for detecting complex sleep disorders.

Who should have a sleep apnea test?
The sleep apnea test is just a part, for which initiation is felt, of the diagnostics for persons showing certain symptoms related to disorders of breathing during sleep. This test is usually recommended when:
- You have symptoms of sleep apnea, such as loud snoring and daytime sleepiness.
- You are at risk for other medical conditions related to sleep apnea.
- Lack of sleep is affecting your quality of life or safety.

What Happens During the Test
During a sleep apnea test, surface electrodes will be attached to your face and scalp to send electrical signals to a monitoring device. These signals, generated by brain and muscle activity, will be recorded digitally. A belt around your chest and abdomen will monitor your breathing patterns, while a pulse oximeter probe, similar to a band wrapped around your finger, will measure your blood oxygen levels.
The indicators to measure in a Sleep Apnea Test
In a sleep apnea test, several key indicators are measured to assess sleep quality and detect respiratory abnormalities. These indicators include:
Airflow
Flow readings are used during tests for sleep apnea to detect abnormal respiration. Airflow in and out of the lungs can be detected by measuring the passage of air with either nasal cannulas or thermistors. Apnea or hypopnea episodes can be detected from such airflow disruptions in the form of pauses or shallow breathing. The measurements taken continuously can indicate how frequent and to what extent such interruptions are taking place and, therefore, diagnose the ailment and arrange treatment.
Oxygen Levels (SpO2)
In the case of the sleep apnea test, an important parameter checked is the saturation of peripheral oxygen in the blood (SpO2). This is generally measured using non-invasive pulse oximetry. It reveals how well the human body maintains its supply of oxygen during sleep, and recurrent low levels of SpO2 indicate apnea events. SpO2 usually remains between 95% and 100% in normal individuals but can be as low as 90% in people suffering from sleep apnea. The measurement of SpO2 is very important in determining how acute a case is and thus what level of treatment it should receive.
Breathing Effort
This is an important indicator that assesses how hard the body is working to breathe during sleep. Monitored through belts placed around the chest and abdomen, breathing effort records the expansion and contraction of these areas. Even when airflow is reduced or halted during apnea episodes, the effort to breathe may still continue. Measuring breathing effort allows healthcare providers to determine the cause of breathing interruptions—whether it is due to obstructive sleep apnea (where effort continues but airflow is blocked) or central sleep apnea (where there is no breathing effort). This distinction is crucial for guiding appropriate diagnosis and treatment.
Heart Rate
In a sleep apnea test, heart rate is an important indicator that reflects cardiovascular health during sleep. Heart rate data is continuously monitored throughout the night, helping healthcare providers assess the heart’s response to breathing and oxygen level changes. Variations in heart rate can indicate cardiovascular stress caused by apnea or hypopnea (shallow breathing). An increased heart rate is often observed during apnea events when oxygen levels drop, while a lower heart rate typically occurs during deeper stages of sleep. Analyzing heart rate patterns enables clinicians to evaluate the severity of sleep apnea and develop an effective treatment plan.
Snoring
This is an important sleep apnea test indicator used to assess the severity of the condition. The occurrence and intensity of snoring are recorded using microphones or sensors, indicating partial obstruction of the airway, which can lead to apneas or hypopneas.
Analyzing the characteristics of snoring—such as its frequency, loudness, and duration—helps healthcare providers correlate snoring with episodes of apnea and determine its impact on overall sleep quality. Understanding the relationship between snoring and breathing disruptions helps clinicians identify effective treatment options. This ultimately improves the patient’s sleep and overall health.
Body Position
In a sleep apnea test, body position plays a chief factor whereby episodes may or may not turn to be severe apneas. The patient’s sleeping position is noted—on their back, side, or stomach since it can affect airway obstruction. Analyzing data on body position alongside other indicators helps healthcare providers gain insights into the application of positional therapy in the treatment plan. This allows them to make personalized recommendations aimed at reducing the frequency and severity of apneas, ultimately improving sleep quality and overall health for the patient.
Apnea-Hypopnea Index (AHI)
The Apnea-Hypopnea Index (AHI) is a crucial measure in sleep apnea testing since it helps quantify the severity of sleep-related breathing disorders. Basically, the AHI speaks to the number of apneas and hypopneas noted per hour of sleep time; in this way, it gives a general pointer of both the state and degree of a patient’s condition.
Purpose of the Sleep Apnea Test
The sleep apnea test is primarily conducted to diagnose sleep-related breathing disorders, such as OSA and CSA. OSA is more prevalent and can lead to numerous serious health consequences. As a result, these tests often focus on this condition.
- The diagnostic process involves measuring breathing patterns during sleep, which helps confirm the presence of respiratory interruptions and assess their frequency and severity. Some tests can also detect other sleep-related disorders or abnormalities.
- The sleep apnea test also plays a crucial role in optimizing sleep apnea treatment methods. A common therapy for OSA is the use of continuous positive airway pressure (CPAP) devices, which deliver a steady stream of air through the nose or mouth to keep the airway open. The test can assist in calibrating the CPAP machine’s pressure, a process known as CPAP titration.
- Additionally, the test can monitor changes in a patient’s breathing patterns over time. Follow-up tests can determine whether the CPAP therapy is effective and assess the impact of weight changes on sleep apnea severity.
Sleep Apnea Test results
The sleep apnea test results provide crucial information about the presence and severity of sleep apnea and related disorders. Here’s an overview of what the results may indicate:
Apnea-Hypopnea Index (AHI)
- Normal: AHI < 5
- Mild Sleep Apnea: AHI 5-15
- Moderate Sleep Apnea: AHI 15-30
- Severe Sleep Apnea: AHI > 30
Oxygen Levels (SpO2)
- Normal Levels: 95% – 100%
- Levels dropping below 90% may indicate serious respiratory issues.
Airflow: Significant reductions or pauses in airflow may indicate episodes of apnea or hypopnea.
Breathing Effort: Continuous effort with little or no airflow suggests obstructive sleep apnea. A lack of effort may indicate central sleep apnea.
Heart Rate: Variations in heart rate may indicate stress on the cardiovascular system due to apnea or hypopnea.
Snoring: Increased snoring may correlate with episodes of apnea or hypopnea.
Body Position: Certain positions (like sleeping on the back) may exacerbate sleep apnea symptoms.
Sleep Stages: Disruptions in sleep stages reflect the impact of sleep apnea on overall sleep quality.
Relationship between sleep apnea test and sleep study
A sleep apnea test is a type of sleep study but is only used to diagnose sleep apnea. In contrast, a sleep study can detect many other types of disorders.
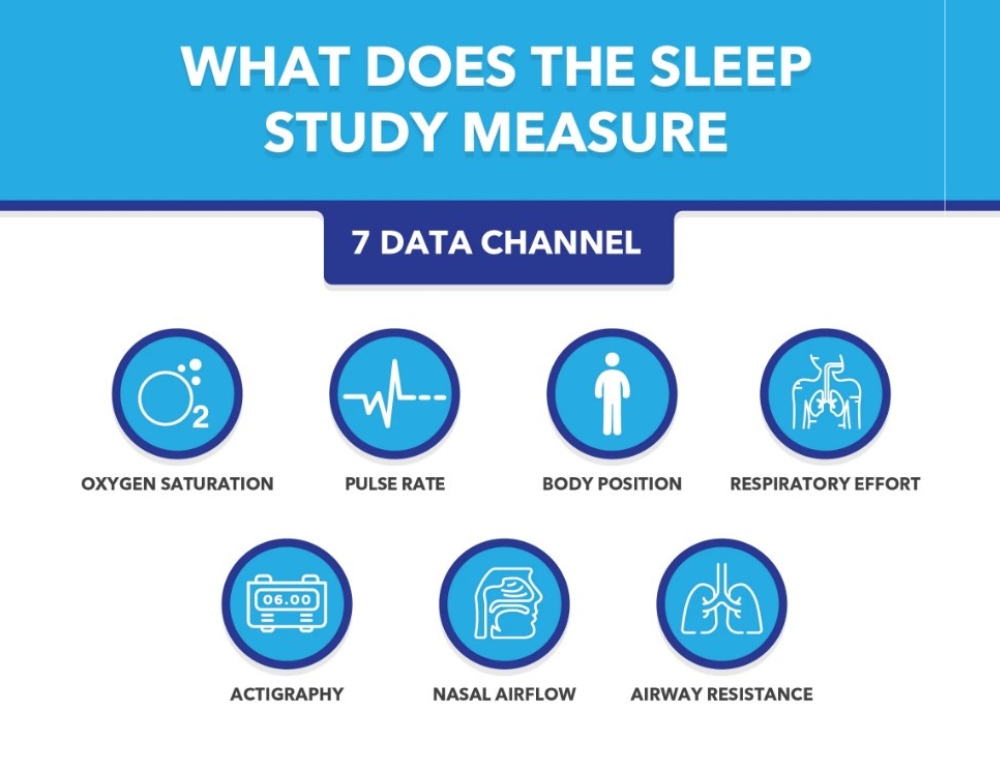
Sleep study (Polysomnography)
Broader scope: A sleep study is a comprehensive test to monitor various factors related to sleep, not just limited to diagnosing sleep apnea.
The monitored indicators: brain waves (EEG), breathing rate, eye movement (REM), heart rate, blood oxygen levels, and muscle movement. It helps detect various sleep disorders, including:
- Sleep apnea
- Insomnia
- Narcolepsy (narcolepsy)
- Restless Legs Syndrome (restless legs syndrome)
- Circadian rhythm sleep disorder
Sleep Apnea Test
Narrower scope: The sleep apnea test primarily focuses on detecting and assessing the severity of sleep apnea. (obstructive sleep apnea – OSA).
The monitored indicators: Breathing rate, blood oxygen level, and the number of apneas or hypopneas during sleep. Does not include more complex indicators such as brain waves or eye movements.
Can be done at home: A sleep apnea test can be conducted at home with simpler equipment. In contrast, a sleep study usually has to be performed at a professional sleep clinic.
Conclusion of the article
Sleep apnea testing is important to diagnose sleep apnea and related sleep disorders. The tests provide information about breathing patterns, oxygen levels, heart rate, and sleep quality. This helps professionals assess the severity and develop an effective treatment plan. Early diagnosis and intervention can prevent serious complications such as cardiovascular disease, daytime fatigue, and cognitive impairment. If you or someone you know has symptoms of sleep apnea, such as loud snoring or excessive sleepiness, seek a sleep study evaluation. Addressing sleep apnea improves sleep quality and enhances overall health and well-being.
Visit our website to explore more about managing sleep disorders and their impact on health. We offer expert resources to help you achieve better sleep at night. At CLM Sleep, we offer comprehensive diagnostic and treatment services for sleep apnea, helping you restore sleep quality and enhance your health. You can also explore other sleep improvement devices at Cpapdiscount.



