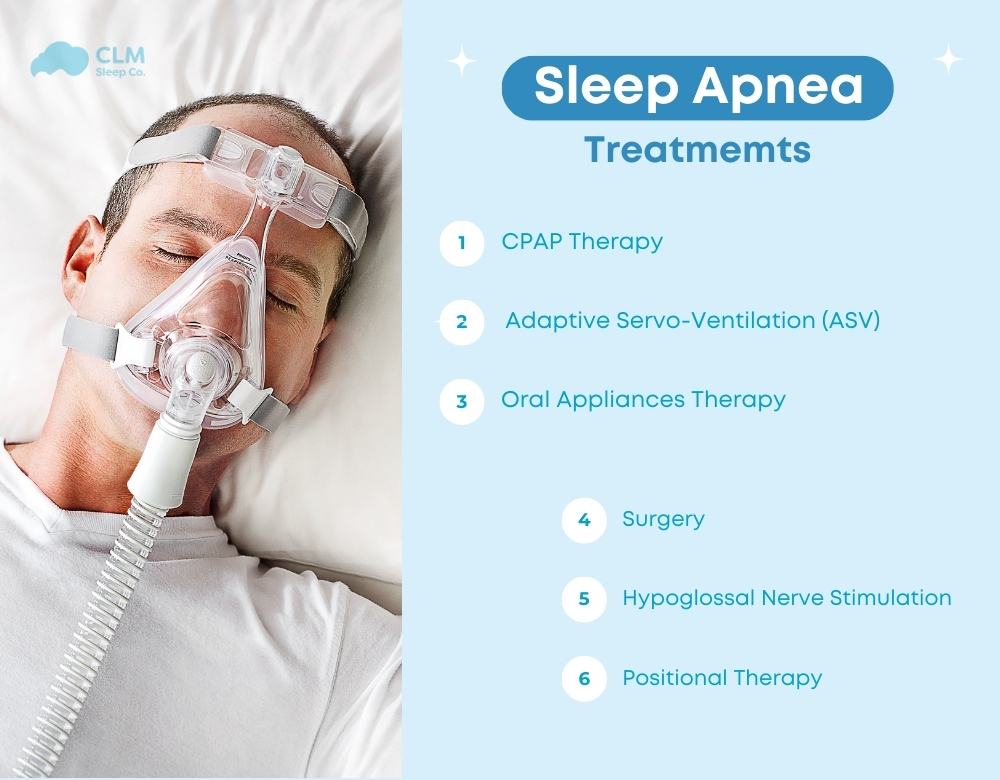
Appropriate sleep apnea treatment will help you improve your health and quality of life. Depending on the type of sleep apnea. rom obstructive sleep apnea (OSA) to central sleep apnea (CSA) or complex sleep apnea (CompSA), there will be different treatment methods. Methods such as CPAP, BiPAP, or more complex therapies like ASV or Diaphragmatic Pacing all aim to maintain a clear and stable airway throughout sleep. Let’s explore in detail with CLM Sleep the mechanisms and suitable candidates for the most effective sleep apnea treatments available today.
Continuous Positive Airway Pressure (CPAP)
Continuous Positive Airway Pressure (CPAP) is a widely used sleep apnea treatment for obstructive sleep apnea (OSA). The CPAP machine provides a continuous stream of air through a mask worn over the nose or both the nose and mouth while you sleep. This airflow has a fixed pressure level, keeping the airway open, helping to prevent airway obstruction and ensuring there is no interruption in breathing. From there, CPAP will help improve sleep, reduce feelings of fatigue and daytime sleepiness, lower the risk of serious conditions such as hypertension, cardiovascular disease, and stroke.

The CPAP machine has three main components:
– Air blower: Creates a continuous airflow with pressure to blow into the airway
– Tube: Transmits air from the air blower to the CPAP mask
– CPAP mask: A device worn over the nose or face to deliver air. There are 3 basic types of masks to suit the preferences and usage habits of each patient, including nasal masks, nasal pillow masks, and full face masks.
See more: How to determine the severity of sleep apnea using the ahi sleep apnea index
Bi-level Positive Airway Pressure (BiPAP)
Bi-level Positive Airway Pressure (BiPAP) is a sleep apnea treatment device for both obstructive sleep apnea and central sleep apnea. It operates similarly to CPAP but with one important difference: BiPAP provides two different air pressure levels, one for inhalation and one for exhalation.
– High inspiratory pressure (IPAP – Inspiratory Positive Airway Pressure): A higher pressure level to assist inhalation and help expand the airways.
– Low expiratory pressure (EPAP – Expiratory Positive Airway Pressure): A lower pressure level during exhalation to reduce airway resistance and make exhalation easier.
The BiPAP machine automatically adjusts between pressure levels throughout the night, depending on each stage of the patient’s respiration. This helps create a more comfortable and pleasant feeling for patients while sleeping, especially for those who have difficulty using CPAP. On the market, BiPAP machines will be larger and more expensive than CPAP machines, so when choosing to purchase, patients need to understand their medical condition and consult with a doctor to make an appropriate choice.
See more: How do BiPAP and CPAP differ?
Adaptive Servo-Ventilation (ASV)
Adaptive Servo-Ventilation (ASV) is an advanced sleep apnea treatment method, particularly effective for patients with central sleep apnea (CSA) or complex sleep apnea. The ASV machine uses sensors to monitor the patient’s breathing rate and blood oxygen levels, helping to detect abnormal changes in breathing, including periods of shallow breathing or apnea.
When signs of apnea or shallow breathing are detected, the ASV machine will automatically adjust the inspiratory pressure (IPAP) and expiratory pressure (EPAP) accurately and promptly, helping to prevent sleep apnea. If the patient breathes normally, the machine will reduce the pressure to ensure comfort, helping the patient maintain a stable and more effective sleep.
The ASV machine provides a flexible and effective treatment solution, helping patients improve sleep quality, reduce fatigue, and lower the risk of sleep apnea-related conditions, especially when other treatments like CPAP or BiPAP are not sufficiently effective.
Oral Appliances Therapy
Oral Appliances Therapy is a non-invasive sleep apnea treatment, particularly effective for mild to moderate obstructive sleep apnea (OSA). This method uses dental appliances to adjust the position of the jaw, tongue, or other structures in the mouth, preventing the muscles and soft tissues in the throat from collapsing and causing airway obstruction, thereby keeping the airway open throughout sleep.

Hypoglossal Nerve Stimulation
Hypoglossal Nerve Stimulation (HGNS) is an advanced method that uses an implantable medical device to stimulate the hypoglossal nerve. When the sensor in the chest wall detects that the patient has started to stop breathing or shows signs of airway obstruction, it will send a signal to the pulse generator, emitting mild electrical pulses to the hypoglossal nerve. To stimulate the sublingual muscles and the throat muscles, causing them to contract, pushing the tongue and soft tissues forward. From there, it improves the airway, reduces sleep apnea symptoms such as snoring, daytime fatigue, and lowers the AHI index, helping to improve sleep quality and reduce the severity of the disease for patients.
The HGNS device consists of three main parts:
– Respiratory sensor: Monitors the patient’s breathing rhythm to detect the moment when stimulation is needed.
– Nerve stimulator: Implanted under the skin, near the hypoglossal nerve
– Pulse generator: Creates small electrical pulses to stimulate the tongue muscles and the muscles in the throat area.
Suitable candidates for HGNS:
– Patients with moderate to severe OSA.
– Those who do not respond well to CPAP or other sleep apnea treatment methods.
– Patients with throat structures unsuitable for airway surgeries.
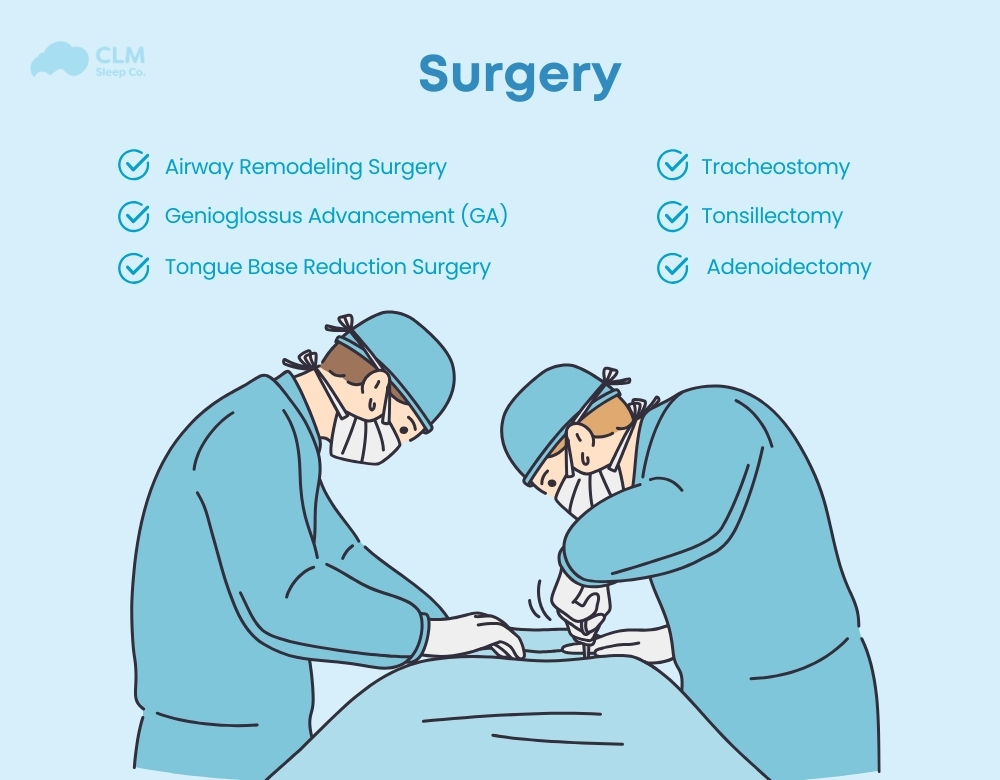
Tonsillectomy or Adenoidectomy
Tonsillectomy and Adenoidectomy is a surgical procedure to remove the tonsils and adenoids, which are tissues of the immune system, with the tonsils located at the back of the throat and the adenoids located behind the nasal cavity. These two methods provide definitive treatment for patients with obstructive sleep apnea due to enlarged tonsils or adenoids, especially in children.
Both procedures are usually performed under general anesthesia and last from 30 to 60 minutes. Tonsillectomy is the removal of the tonsils through an incision at the back of the throat. Adenoidectomy removes the adenoids through the mouth or nasal cavity, depending on the surgical method.
Surgery
Surgery is an effective sleep apnea treatment method for patients with obstructive sleep apnea (OSA) who do not respond well to non-surgical treatments such as CPAP or other supportive devices. Some specific surgeries aim to expand the upper airway, improve airflow, and reduce the risk of obstruction.
Airway Remodeling Surgery
Airway Remodeling Surgery aims to change the structure of tissues or bones in the upper respiratory tract to reduce airway obstruction.
– Uvulopalatopharyngoplasty (UPPP): Removal of excess soft tissue in the throat area, including the uvula, part of the soft palate, and surrounding tissue. This procedure helps to widen the airway in the throat area and reduce the risk of obstruction. This method helps reduce snoring, suitable for patients with mild to moderate sleep apnea. More effective when combined with other treatment methods such as CPAP.
– Maxillomandibular advancement (MMA) is a complex procedure, a surgery that pushes the upper and lower jaw forward, creating more space for the airway behind. This method significantly expands the upper airway, improves airflow, and reduces the number of apneas. Suitable for patients with severe OSA or those with jaw structure abnormalities. Note, this surgical method should be indicated after a thorough assessment of the patient’s condition and anatomical structure.
Genioglossus Advancement (GA)
Genioglossus Advancement (GA) is a surgical procedure in the mandible to treat obstructive sleep apnea (OSA). The primary goal is to prevent the tongue from falling back during sleep, reducing the risk of airway obstruction. Performed under general anesthesia, the procedure involves making a small incision inside the mouth, near the gums, to move the attachment of the base of the tongue forward. This adjustment stabilizes the tongue and keeps the airway clear. Often combined with surgeries like UPPP or Maxillomandibular Advancement, enhances overall sleep apnea treatment effectiveness.
The suitable candidates for GA will be:
– Patients with moderate to severe OSA.
– Those with tongue structures that obstruct the airway.
– Patients do not respond well to CPAP or other treatment methods.
Tongue Base Reduction Surgery
Tongue Base Reduction Surgery is a surgical procedure aimed at reducing the size of the tongue muscle to treat obstructive sleep apnea. (OSA). The patient will be under general anesthesia throughout the surgery. The doctor makes a small incision at the back of the mouth or throat to access the base of the tongue. To remove or reduce excess tissue at the base of the tongue using tools such as lasers or radio waves. The suitable candidates for this method are
– Patients with moderate to severe obstructive sleep apnea who do not respond well to non-surgical treatments such as CPAP
– Individuals with an enlarged tongue base causing airway obstruction
– Those who cannot undergo other surgical methods such as UPPP or Maxillomandibular Advancement (MMA)
Tracheostomy
Tracheostomy is a major invasive surgical procedure and will be the last resort for cases of severe, chronic, life-threatening sleep apnea. This method will create a direct passage into the trachea (throat) through the neck to establish an alternative airway. After anesthesia, the surgeon will make a small incision in the neck area, usually below the Adam’s apple, and create an opening into the trachea. A tube will be inserted into this opening to keep the airway clear, allowing air to go directly into the lungs, bypassing the upper airway. When performing this procedure, the patient needs to be continuously monitored to avoid the risk of infection and complications.
Inspire Therapy
Inspire Therapy is quite similar to the Hypoglossal Nerve Stimulation method, which also uses an implanted device to stimulate the muscles of the airway, keeping the airway open throughout sleep. But it has a more complex structure and the ability to automatically adjust the level of nerve stimulation, instead of having to manually adjust it like the HGNS method.
The implantable device of this method includes:
A small pulse generator implanted under the skin in the chest, usually near the collarbone.
The respiratory sensor is placed on the chest to monitor the patient’s breathing patterns while sleeping.
The stimulating wire connects to the hypoglossal nerve, controlling tongue movement.
How It Works: The patient will activate the device using a small remote control before going to sleep. When the pulse generator detects that the patient has stopped breathing or has reduced airflow, it will send a mild stimulation pulse to the hypoglossal nerve, causing the tongue and throat muscles to contract, helping to open the airway. The Inspire device has the ability to adjust the stimulation level, depending on the patient’s respiratory needs during each sleep cycle.
Oxygen therapy
Oxygen therapy is a sleep apnoea treatment method that involves delivering additional oxygen to patients who experience low oxygen levels in their blood during sleep. This is commonly used for individuals with sleep apnea, particularly those with central sleep apnea (CSA) or complex sleep apnea (CompSA), where oxygen levels may drop due to irregular breathing patterns. Oxygen therapy helps maintain optimal oxygen saturation levels, improving overall oxygen delivery to vital organs during sleep.
The therapy can be administered through a nasal cannula, face mask, or other devices depending on the patient’s needs and the severity of their condition. It is often used in conjunction with other treatments like CPAP or BiPAP to provide comprehensive care for patients with sleep apnea.
Diaphragmatic pacing
Diaphragmatic pacing will be similar to the HGNS and Inspire Therapy methods in that they both involve implanting a sensor device into the body and using electrical impulses to stimulate the muscles. But the sensor device of Diaphragmatic pacing will be implanted near the diaphragm or the vagus nerve. To maintain a stable breathing rhythm for patients with central sleep apnea (CSA) or complex sleep apnea (CompSA).
Positional Therapy
Positional Therapy focuses on changing sleeping positions, from lying on the back to lying on the side or elevating the head to reduce airway obstruction. To maintain the correct sleeping position, some supportive methods can be used, such as a backpack, posture correction devices, or active sleeping positions. This method is particularly effective for patients with mild to moderate obstructive sleep apnea, especially due to sleeping posture.
Medications
Medications are not a complete sleep apnea treatment, but they can support other treatment methods such as CPAP or surgery. Some medications help control the side symptoms of sleep apnea, such as excessive daytime sleepiness, while others treat related issues, such as nasal congestion. The selection and use of medication should be prescribed and ordered by a doctor.
Lifestyle Changes
Weight Loss
Studies show that weight loss can significantly reduce the symptoms of sleep apnea. When losing weight, the fat around the neck and chin will decrease, thereby reducing pressure on the airways, which helps improve sleep quality and supports sleep apnea treatment, especially obstructive sleep apnea.
Changing Sleep Position
The sleeping position directly affects the breathing mechanism during sleep. People with sleep apnea should try to sleep on their side or with their head elevated to help naturally open the airways and reduce the risk of obstruction. When sleeping, you should avoid lying on your back, as this position can cause the tongue and soft tissues in the throat to easily fall back, obstructing the airway.
Avoiding Alcohol and Sedatives
Alcohol and sedatives can reduce the ability of the throat muscles, including those that control the airway, to contract. When these muscles are overstretched, the airways are prone to collapse, increasing the risk of airway obstruction and making breathing difficult. Additionally, alcohol and sedatives inhibit the central nervous system, disrupting signals from the brain to the respiratory control organs, making CSA symptoms even more severe. Therefore, limiting or avoiding alcohol and sedative medications will help in reducing symptoms and improve sleep apnea treatment.
Quitting Smoking
Smoking is the cause of inflammation and irritation of the respiratory mucosa, leading to increased mucus secretion and narrowing of the airways. Smoking will make breathing difficult, air circulation will be hindered, increasing the risk of obstruction and sleep apnea. Quitting smoking helps reduce inflammation, keeps the airways clearer, and improves breathing during sleep.
Treatment Options for Different Types of Sleep Apnea
Each treatment method is designed to address the different causes and symptoms of sleep apnea, ranging from mild to severe. Below are the treatment methods suitable for each type of sleep apnea.
Treatments for OSA
The sleep apnoea treatment methods for obstructive sleep apnea focus on opening the airway and addressing the issues that cause airway obstruction, helping patients breathe easily and steadily throughout the night.
- Continuous Positive Airway Pressure (CPAP)
- Bi-level Positive Airway Pressure (BiPAP)
- Adaptive Servo-Ventilation (ASV)
- Oral Appliances Therapy
- Surgery: Uvulopalatopharyngoplasty, Maxillomandibular Advancement, Genioglossus Advancement
- Inspire Therapy
Treatments for CSA
CSA treatment focuses on addressing the issue of disrupted breath control. As the brain’s respiratory control center does not send proper signals to the diaphragm and respiratory muscles. Common treatment methods include:
- Adaptive Servo-Ventilation (ASV)
- Bi-level Positive Airway Pressure (BiPAP)
- Medications (e.g., Theophylline)
- Oxygen therapy
- Diaphragmatic pacing
Treatments for CompSA
CompSA treatment requires a complex and flexible sleep apnea treatment regimen, combining various methods, and can utilize most OSA and CSA treatment methods. These methods can be adjusted or combined depending on the condition and stage of the disease. Therefore, patients need to be much more persistent and make greater efforts to achieve quality and stable sleep.
Conclusion of the article
Sleep apnea is a serious condition that can significantly affect the quality of life and overall health. Different types of sleep apnea require different sleep apnea treatment methods. The choice of treatment method will depend on the symptoms and underlying cause of the condition. When you notice symptoms of sleep apnea, you need to see a doctor for diagnosis and to receive appropriate treatment. At CLM Sleep, we offer comprehensive diagnostic and treatment services for sleep apnea. Helping you restore sleep quality and enhance your health. You can also explore other sleep improvement devices at Cpapdiscount.