Central sleep apnea (CSA) is a rare type of sleep apnea, accounting for only about 5% of all cases. This disease is somewhat more complex and difficult to treat than OSA, because it involves the brain and nervous system. This condition can lead to fragmented sleep, reduced oxygen levels, and other health complications. Understanding the causes, symptoms, and treatment options for central sleep apnoea is crucial for managing this condition and improving overall health and quality of life.
Central sleep apnea overview
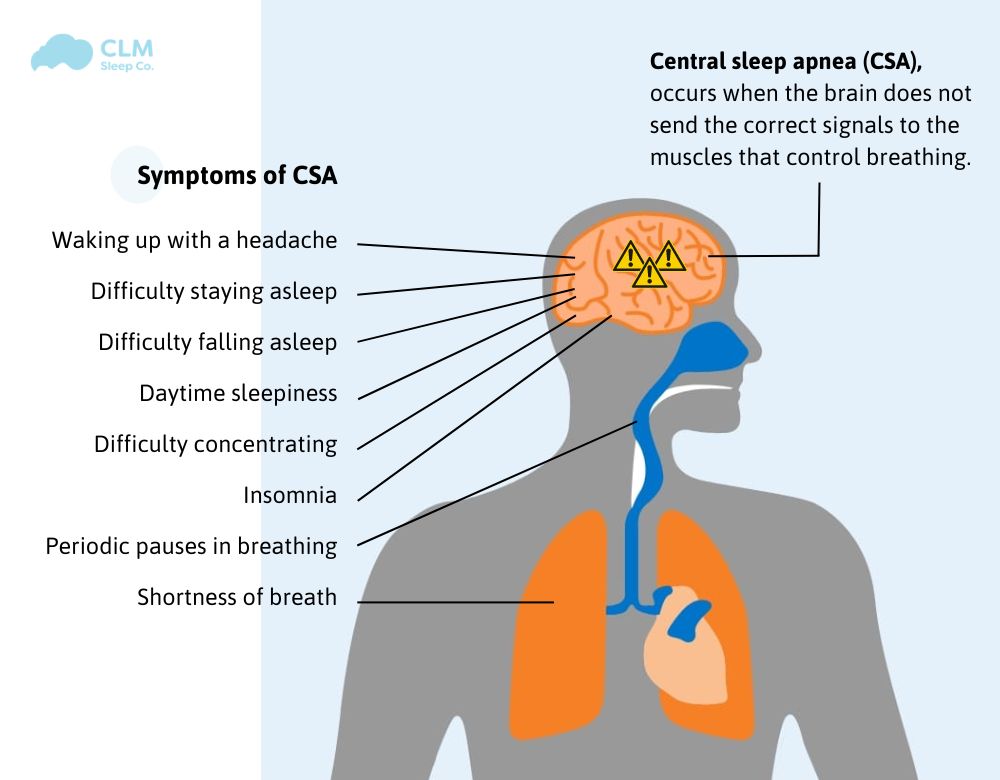
Central sleep apnea (Central sleep apnoea – CSA) is a complex sleep disorder due to a lack of signals from the brain, in which breathing is interrupted, repeatedly stopping and starting during sleep. The brain fails to send the proper signals to the muscles that control breathing, causing breathing to stop intermittently. Some episodes of apnea can last for a few seconds, others can last for tens of seconds or even minutes, depending on the severity.
This type of sleep apnea often affects people with underlying medical conditions such as heart failure or stroke. CSA will cause you to wake up suddenly, accompanied by difficulty breathing, insomnia, excessive daytime sleepiness, difficulty concentrating and poor mood. In the long term, it will affect quality of life and lead to other serious health problems
See more: Apnea Meaning
What are the types of central sleep apnea?
CSA is divided into six categories:
Primary CSA: A rare form without an underlying cause.
Cheyne–Stokes respiration: A pattern of breathing often seen in heart failure patients.
High-altitude periodic breathing: Triggered by reduced oxygen levels at high altitudes.
CSA due to a medical condition without CSB: Linked to certain health conditions.
CSA due to a medication or substance: Induced by specific drugs or substances.
Treatment Emergent Central Apnea: Occurs when obstructive sleep apnea treatment leads to CSA.What is the difference between central sleep apnoea and obstructive sleep apnoea?
The key difference between central sleep apnea and obstructive sleep apnea lies in their causes. Central sleep apnea is due to a failure in the brain’s signal transmission to the muscles that control breathing, while obstructive sleep apnea is caused by a physical blockage of the airway. In CSA, there is no effort to breathe during pauses, whereas, in obstructive sleep apnea, the body struggles to breathe against the blocked airway.
Symptoms and Causes
Symptoms of Central Sleep Apnoea
The symptoms of central sleep apnea can vary depending on the underlying cause. However, some common signs include:
- Frequent waking up gasping for air
- Daytime sleepiness
- Difficulty concentrating
- Fatigue
- Irritability
- Headaches
- Heart palpitations
- Chest pain
See more: Can You Have Sleep Apnea Without Snoring?
Signs of the 6 categories of central sleep apnea:
Primary CSA: Symptoms may include frequent waking up gasping for air, daytime sleepiness, and fatigue.
Cheyne-Stokes respiration: This is characterized by periods of rapid, shallow breathing followed by periods of apnoea.
High-altitude periodic breathing: This occurs at high altitudes and is characterized by periods of rapid, shallow breathing followed by periods of apnea.
CSA due to a medical condition without CSB: The symptoms may vary depending on the underlying medical condition.
Central sleep apnea due to a medication or substance: The symptoms may vary depending on the medication or substance.
Treatment Emergent Central Apnea: This is a sudden onset of central sleep apnea that occurs during treatment for another condition.
When to see a doctor
If you experience any of the symptoms listed above, it’s important to see a doctor for evaluation. Early diagnosis and treatment can help prevent serious health complications.
Causes of Central Sleep Apnoea
Central sleep apnea occurs when the brain fails to send proper signals to the muscles that control breathing. This can be caused by a variety of factors, including:
Underlying medical conditions: Heart failure, stroke, neurological disorders (such as Parkinson’s disease or amyotrophic lateral sclerosis), kidney failure, and certain hormonal imbalances can all contribute to central sleep apnoea.
Medication use: Opioids, sedatives, and certain blood pressure medications can increase the risk of central sleep apnea.
High altitude: Sleeping at high altitudes can disrupt the body’s breathing patterns and lead to central sleep apnea.
Aging: As people get older, their brains may become less efficient at regulating breathing during sleep.
Congenital conditions: Some people are born with conditions that affect the brain’s control of breathing, such as Rett syndrome or Prader-Willi syndrome.
Treatment-emergent central sleep apnea: This occurs when people who are already being treated for obstructive sleep apnoea with CPAP develop central sleep apnea as a side effect of the treatment.
It’s important to note that in some cases, the exact cause of central sleep apnoea may remain unknown.
Risk factors of CSA
The risk factors for Central Sleep Apnea (CSA) include a variety of health conditions, lifestyle factors, and external influences. Here are some of the key risk factors:
Heart Conditions:
- Heart Failure: CSA is commonly associated with heart failure, particularly in cases of reduced heart function, where the heart cannot effectively pump blood, leading to abnormal breathing patterns.
- Atrial Fibrillation: Irregular heartbeats can affect breathing control during sleep, increasing the risk of CSA.
Stroke or Brain Injury: Damage to the brainstem, which controls breathing, can result in CSA. Stroke survivors and individuals with brain injuries are at higher risk.
Age: CSA is more prevalent in older adults, particularly those over the age of 60, as aging can weaken the brain’s control over breathing.
Gender: Men are more likely to develop CSA than women, although the risk increases for women after menopause.
High-Altitude Exposure: Spending time at high altitudes, where oxygen levels are lower, can trigger CSA, especially if the exposure is prolonged.
Medications: Certain medications, particularly opioids, sedatives, and narcotics, can depress the central nervous system, leading to CSA.
Chronic Lung Diseases: Conditions such as chronic obstructive pulmonary disease (COPD) can contribute to CSA by affecting normal respiratory function.
Kidney Failure: People with chronic kidney disease, particularly those on dialysis, may have an increased risk of developing CSA due to fluid imbalances and related factors.
Obstructive Sleep Apnea (OSA) Treatment: Some individuals who are treated for obstructive sleep apnea (OSA) with devices like CPAP may develop treatment-emergent central sleep apnea (TECSA).
Understanding these risk factors can help in the early identification and management of Central Sleep Apnea, potentially improving outcomes for those affected
See more: Is sleep apnea hereditary?
Complications
Central Sleep Apnoea (CSA) can lead to several complications if left untreated or poorly managed. These complications can significantly impact a person’s overall health and quality of life. Here are the main complications associated with CSA:
Cardiovascular Problems
- High Blood Pressure: Repeated drops in blood oxygen levels during sleep can cause hypertension, leading to long-term cardiovascular strain.
- Heart Failure: CSA is both a symptom and a risk factor for heart failure, creating a vicious cycle that can worsen both conditions.
- Arrhythmias: Irregular heartbeats, including atrial fibrillation, can occur due to the intermittent lack of oxygen, increasing the risk of stroke and other heart issues.
Excessive Daytime Sleepiness
Frequent interruptions in sleep due to apnea can lead to chronic fatigue, excessive daytime sleepiness, and a decreased ability to concentrate. This can affect productivity, mood, and overall quality of life.
Cognitive Impairment
Lack of restful sleep and repeated drops in oxygen can lead to memory problems, difficulty concentrating, and other cognitive impairments over time.
Increased Risk of Accidents
Due to excessive daytime sleepiness and impaired concentration, individuals with CSA are at a higher risk of accidents, particularly while driving or operating machinery.
Metabolic Disorders
CSA can contribute to metabolic issues like insulin resistance, increasing the risk of developing type 2 diabetes.
Pulmonary Hypertension
Chronic low oxygen levels can lead to elevated blood pressure in the lungs, known as pulmonary hypertension, which can strain the right side of the heart.
Impaired Quality of Life
The combined effects of fatigue, cognitive difficulties, and cardiovascular issues can lead to a significant decline in overall quality of life, affecting work, social interactions, and emotional well-being.
Worsening of Underlying Conditions
For patients with pre-existing conditions like heart failure or stroke, CSA can exacerbate these issues, making them more difficult to manage.
Recognizing and treating central sleep apnea is crucial to prevent these complications and improve the patient’s overall health and well-being.
Diagnosis and Treatment
Diagnosis and Tests
Diagnosing central sleep apnea (CSA) typically involves a combination of clinical evaluation, sleep studies, and other diagnostic tests. The diagnosis is confirmed using polysomnography, monitoring breathing, heart rate, and brain activity while you sleep. This is a comprehensive sleep study that monitors various physiological parameters during sleep. The specific criteria and figures used to diagnose CSA can vary, but generally, a diagnosis is made based on:
Apnea-hypopnea index (AHI): This measures the number of times your breathing stops or slows significantly per hour of sleep. A diagnosis of CSA is often made if the AHI is above 5, with at least 50% of the events being central apneas.
Oxygen desaturation index (ODI): This measures how often your blood oxygen level drops significantly during sleep.
Central apnea percentage: This indicates the percentage of apneas that are central in nature, rather than obstructive.
How to central sleep apnea test at home?
While a formal sleep study is the most accurate way to diagnose CSA, there are some at-home tests that can provide preliminary information. These include:
At-home sleep apnea monitors: These devices can track your breathing and snoring patterns, but they may not be as accurate as a sleep study.
Sleep diaries: Keeping a sleep diary can help you identify potential symptoms of CSA, such as excessive daytime sleepiness or waking up gasping for air.
Detailed Overview of the Six Categories of Central Sleep Apnea (CSA)
Central Sleep Apnea (CSA) is categorized into six distinct types, each with its own causes, characteristics, and implications for treatment. Here’s a detailed overview of each category:
Primary Central Sleep Apnea
- Description: Also known as idiopathic CSA, this type occurs without any identifiable underlying cause. It’s rare and primarily seen in older adults.
- Characteristics: Primary CSA is marked by frequent pauses in breathing during sleep without any associated medical condition or external trigger. It is often diagnosed when other potential causes have been ruled out.
Cheyne–Stokes Respiration (CSR)
- Description: Cheyne–Stokes respiration is a specific pattern of breathing characterized by a gradual increase and then decrease in breathing effort followed by a period of apnea (no breathing). It’s often associated with heart failure or stroke.
- Characteristics: This type of CSA is commonly seen in patients with congestive heart failure or neurological conditions. The waxing and waning breathing pattern can be particularly disruptive to sleep and is often accompanied by a decrease in blood oxygen levels.
High-Altitude Periodic Breathing
- Description: This form of CSA occurs in individuals exposed to high altitudes, typically above 8,000 feet (2,500 meters), where oxygen levels are significantly lower.
- Characteristics: At high altitudes, the reduced oxygen levels can lead to periodic breathing patterns, with cycles of deep breaths followed by shallow breaths or pauses. This type is usually temporary and resolves when the individual returns to lower altitudes.
CSA Due to a Medical Condition Without Cheyne–Stokes Breathing
- Description: This category includes CSA associated with medical conditions such as Parkinson’s disease, brainstem lesions, or neuromuscular disorders, but without the Cheyne–Stokes breathing pattern.
- Characteristics: Patients with this type of CSA may experience regular pauses in breathing due to the underlying medical condition that affects the brain’s control over breathing.
Central Sleep Apnea Due to a Medication or Substance
- Description: Certain medications or substances can depress the central nervous system, leading to CSA. Opioids, sedatives, and certain anesthetics are common culprits.
- Characteristics: In this category, the apnea is directly linked to the use of drugs that affect the brain’s ability to regulate breathing. Reducing or discontinuing the medication often resolves the apnea.
Treatment-Emergent Central Sleep Apnea (TECSA)
- Description: Also known as complex sleep apnea, TECSA occurs when obstructive sleep apnea (OSA) is treated, usually with continuous positive airway pressure (CPAP) therapy, but central apneas emerge as a result.
- Characteristics: In TECSA, central apneas appear after the airway obstruction is resolved, often complicating the treatment process. It’s believed that the sudden change in breathing patterns due to OSA treatment triggers the central apneas.
Each of these categories highlights the diverse nature of central sleep apnea and underscores the importance of precise diagnosis for effective treatment. Understanding the specific type of CSA is crucial in determining the best course of action to manage the condition and improve sleep quality.
Management and Treatment
Managing and treating central sleep apnea involves addressing the underlying causes and utilizing specific interventions to improve breathing during sleep. The treatment for CSA often involves a combination of medical interventions and lifestyle changes.
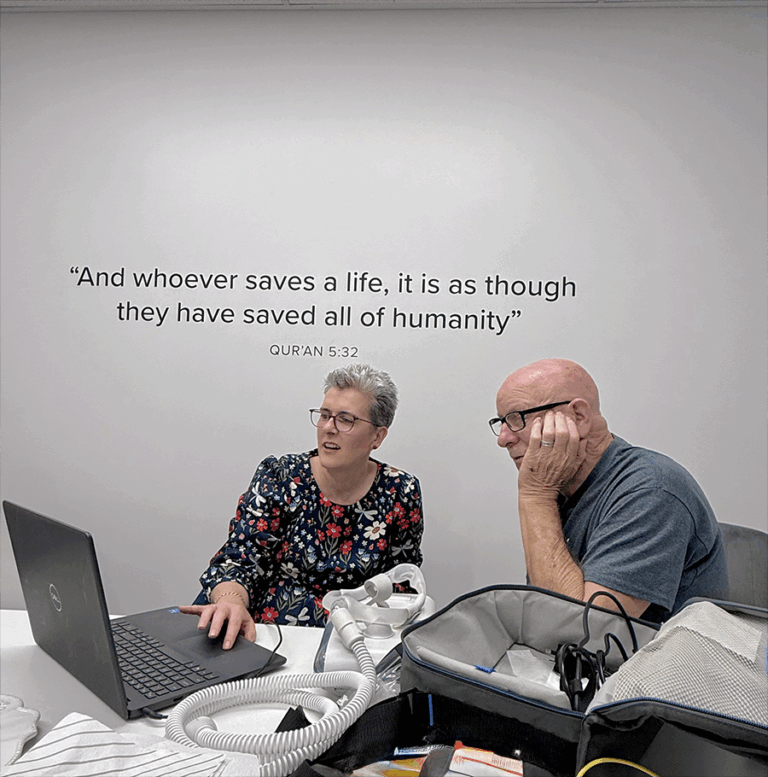
Continuous Positive Airway Pressure (CPAP) machines are commonly used to treat CSA by providing a steady flow of air through a mask, which helps maintain an open airway and stabilizes breathing. For some patients, adaptive servo-ventilation (ASV) or bilevel positive airway pressure (BiPAP) machines may be more effective. These devices adapt to the individual’s breathing pattern and provide more targeted support.
In addition to these mechanical treatments, lifestyle modifications play a vital role in managing CSA. This includes weight management, avoiding alcohol or sedatives before bedtime, and establishing a regular sleep schedule. For those seeking personalized advice and treatment, our clinic offers specialized services tailored to each patient’s needs, including CPAP machine fittings and ongoing support.
See more: Untreated sleep apnea life expectancy
Departments and Specialties
Departments that treat central sleep apnea
Pulmonology: Focuses on respiratory health and the mechanics of breathing.
Neurology: Addresses the brain’s role in controlling breathing.
Sleep Medicine: Specializes in diagnosing and treating various sleep disordered breathing, including central sleep apnea.
Otolaryngology: Specializes in the diagnosis and treatment of ear, nose, and throat disorders, which can sometimes contribute to sleep apnea.
Central sleep apnea treatment specialist
A sleep medicine specialist is typically the most qualified professional to diagnose and treat central sleep apnea. They have specialized training in sleep disorders and can recommend appropriate treatment options.
Prevention
Preventing central sleep apnea (CSA) largely revolves around managing risk factors and underlying conditions that can contribute to its development. While there is no guaranteed way to prevent CSA, several strategies can reduce the likelihood or severity of the condition:
Manage Underlying Health Conditions: Treating heart failure, stroke, or other neurological disorders can lower the risk of CSA.
Avoid Alcohol and Sedatives: These substances can affect brain signaling and worsen apnea events. Limiting or avoiding them, especially before bedtime, can help.
Quit smoking: Nicotine in cigarettes can affect the respiratory center in the brain, reducing the ability to regulate breathing and increasing the risk of apnea.
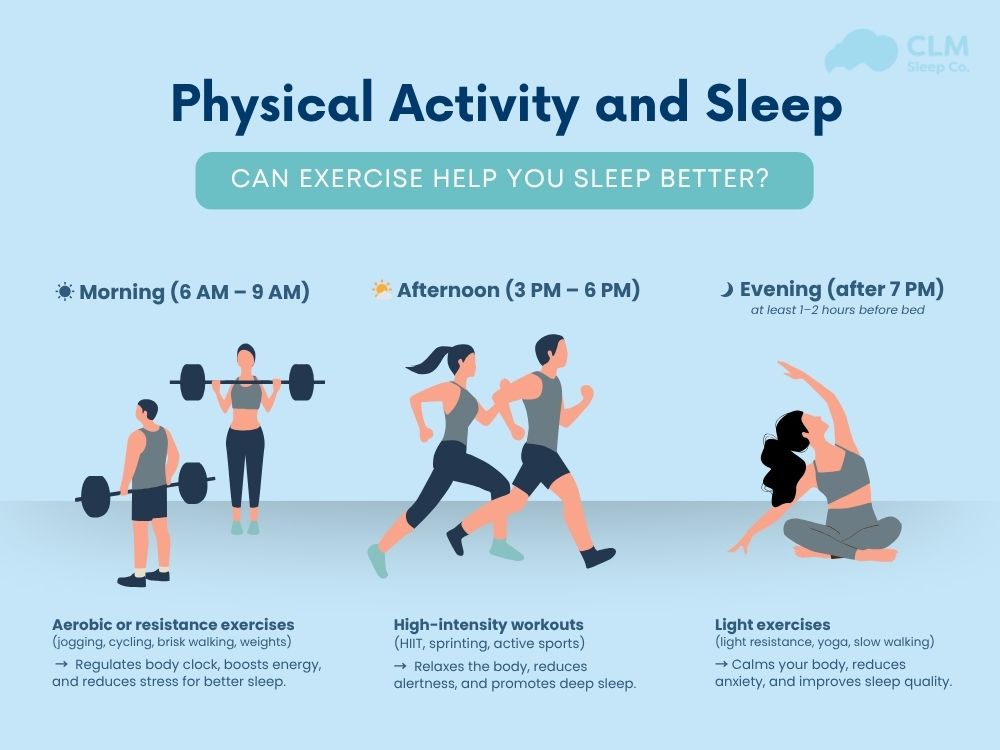
Maintain a Healthy Weight: Obesity can exacerbate breathing disorders, including CSA. Weight loss through a balanced diet and regular exercise may prevent the onset or progression of CSA.
Follow a Regular Sleep Schedule: Consistent sleep patterns can support overall sleep quality and reduce the likelihood of apnea events.
Outlook / Prognosis
The prognosis for individuals with central sleep apnea varies based on the underlying cause, the severity of the condition, and the effectiveness of the treatment plan. With proper management, many people can experience significant improvements in symptoms and overall quality of life.
Effective Treatments: Use of CPAP, ASV, or BiPAP machines, combined with lifestyle modifications and treatment of underlying conditions, can lead to a reduction in apnea events and improved sleep quality.
Long-Term Management: Some cases of CSA are chronic and require ongoing management. Regular follow-ups with healthcare providers are crucial to monitor progress and adjust treatment plans as needed.
Complications: If left untreated, CSA can lead to serious complications such as cardiovascular problems, cognitive impairments, and reduced life expectancy. Early diagnosis and treatment are essential for better outcomes.
Living with central sleep apnea
Living with central sleep apnea requires a comprehensive approach that includes lifestyle adjustments, medical management, and ongoing support:
Adhering to Treatment Plans: Using prescribed devices like CPAP machines consistently is key to managing symptoms and improving sleep quality.
Regular Check-ups: Regular visits to a sleep specialist or pulmonologist can help in adjusting treatment and managing any side effects from therapy.
Lifestyle Changes: Incorporating healthy habits such as regular exercise, a balanced diet, and good sleep hygiene can complement medical treatments.
Support Systems: Joining support groups or consulting with sleep apnea specialists can provide emotional support and practical tips for managing CSA.
Access to Services: At our clinic, we offer a range of services, including personalized treatment plans, CPAP machine adjustments, and ongoing patient education to help individuals live well with central sleep apnea.
These sections provide comprehensive and informative content, effectively using the keyword “central sleep apnea” while addressing prevention, prognosis, and daily management.
See more: Effective Ways to Heal Sleep Apnea Naturally for Better Health
Conclusion of the article
Compared to obstructive sleep apnea, central sleep apnea is little more complicated. Surgery and other supplementary treatment options are required since it affects the nerve system and brain. Thus, prompt diagnosis and treatment will guarantee life quality, avoid complications, and support long-term health. If you find yourself experiencing some of the signs mentioned above, please talk to your personal doctor or visit CLM Sleep for consultation, diagnosis, and treatment using the latest methods available today.