Narcolepsy is a chronic disease that disrupts life’s natural course by creating difficulties with maintaining wakefulness during the day. People often experience excessive daytime sleepiness without warning-which could even be accompanied by hallucinations and transient paralysis. To many people living with it, getting to know this condition is essential and promoting information about its effect on daily life and ways to manage it in the best possible way. In this article, CLM Sleep will reveal the causes, symptoms, and narcolepsy treatment approaches that will take you to the first steps to improve your sleep health.
What is Narcolepsy?
Below is basic information about Narcolepsy:
Definition and General Concepts
What does narcolepsy meaning? Narcolepsy is a chronic neurological disorder caused by dysfunction within the brain mechanisms that control the cycle of sleep and waking. Patients with narcolepsy are usually refreshed in the morning; however, they often complain of marked excessive daytime sleepiness, tiredness being the main complaint. Many patients have disturbed nocturnal sleep and have difficulty maintaining sleep for a prolonged period.
Under normal circumstances, the sleep cycle switches into rapid eye movement (REM) sleep approximately 60-90 minutes after onset. REM sleep is the stage during which most dreaming takes place, and the brain transiently inhibits the motor systems from enacting the dreams and prevents their actualization.
In narcolepsy, the regulation of sleep and wakefulness is faulty which leads to mixed and broken sleep. The boundary between being awake and asleep becomes vague; a mixture of these states occurs. Typically, individuals with narcolepsy go rapidly into REM sleep; often, within 15 minutes of falling asleep. They may also experience episodes of REM-related muscle weakness, or phenomena that are dream-like when they are awake.
Narcolepsy can have quite a profound impact on daily life overall, and if not diagnosed and treated well, it might interfere with emotional health, social relationships, and performance of mental functions including work and school.

Types of Narcolepsy
Narcolepsy is divided into two main types:
- Type 1 Narcolepsy: What are narcolepsy and cataplexy symptoms? Previously known as narcolepsy with cataplexy, this type is diagnosed in one of two ways. The first method involves detecting low levels of hypocretin (also called orexin), a brain chemical that regulates wakefulness and REM sleep. The second method is identifying the presence of cataplexy – sudden episodes of muscle weakness – along with excessive daytime sleepiness, confirmed through a specialized nap test.
- Type 2 Narcolepsy: Formerly referred to as narcolepsy without cataplexy, this type is characterized by excessive daytime sleepiness without episodes of cataplexy. Generally, symptoms are milder, and patients have normal hypocretin levels. Sometimes, secondary narcolepsy can develop after a head injury that damages the hypothalamus – a region of the brain that regulates sleep. In this case, patients may display narcoleptic symptoms as well as severe neurological problems and an unusually extended night sleep duration (more than 10 hours)
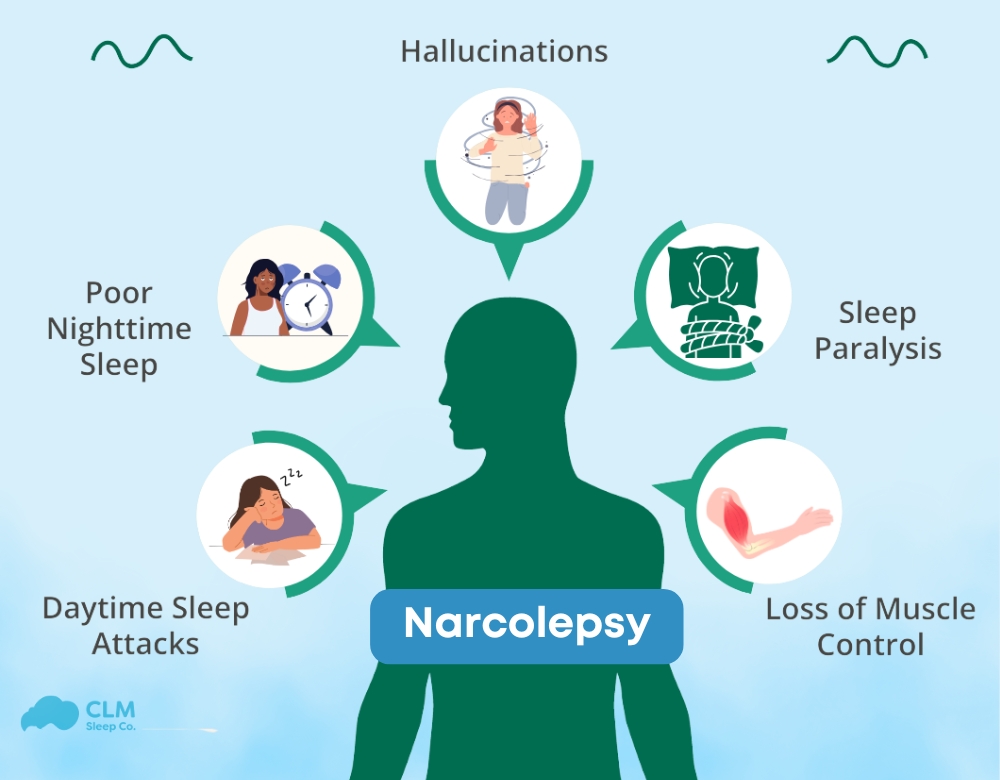
Common Symptoms of Narcolepsy
Once narcolepsy develops, it becomes a lifelong condition. Narcolepsy symptoms vary among individuals and may improve over time but will never fully disappear. Despite the severity of symptoms, narcolepsy does not lead to permanent dysfunction. Following an episode, individuals quickly regain the ability to move and speak.
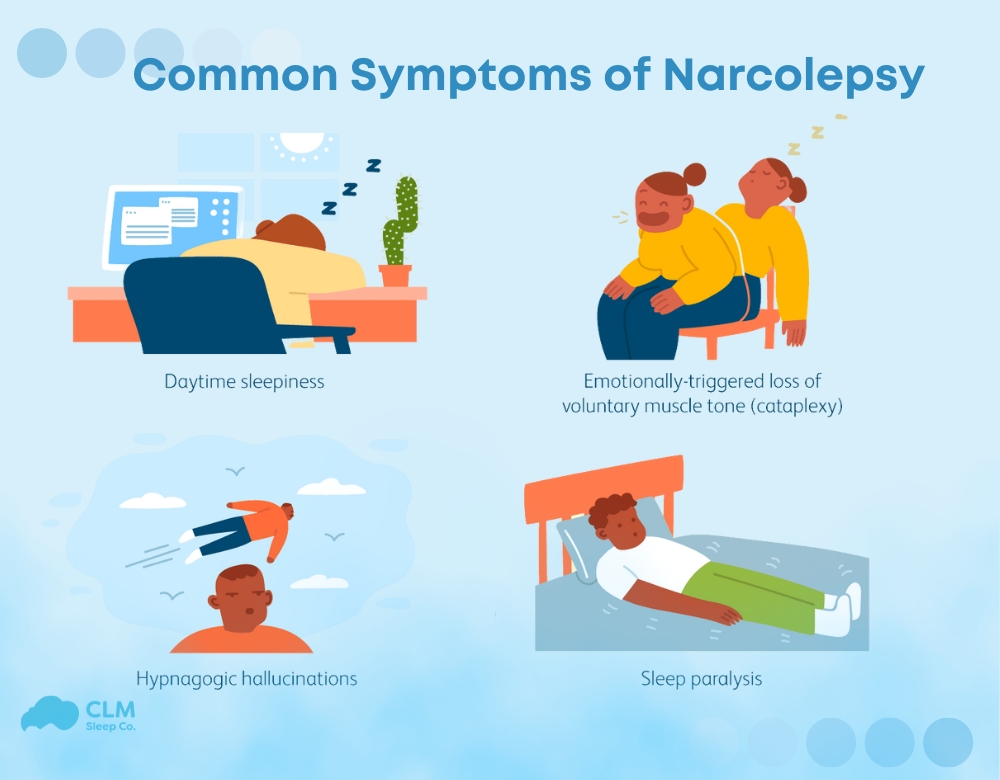
The most common narcolepsy symptoms include:
Excessive Daytime Sleepiness (EDS)
All patients with narcolepsy suffer from EDS, often the presenting complaint. All patients with narcolepsy have some degree of EDS, but the severity varies. EDS can produce irresistible sleep attacks throughout the day, even after adequate nocturnal sleep. Sleep tendency is often characterized by the occurrence of sudden, irresistible sleep episodes. Patients may remain asymptomatic between such attacks, particularly if they are engaged in stimulating activities.
Cataplexy
Cataplexy involves sudden muscle weakness triggered by strong emotions such as laughter, fear, anger, or excitement. It may develop weeks or years after EDS onset. Some individuals experience only one or two episodes in their lifetime, while others face multiple attacks daily. In about 10% of cases, cataplexy is the first symptom. Often misdiagnosed as a seizure disorder, cataplexy episodes can range from mild (minor muscle weakness) to severe (total body collapse). Even in severe cases, individuals remain fully conscious but are temporarily unable to move, speak, or open their eyes. These episodes, lasting seconds to minutes, are not dangerous if the person is in a safe environment.
Sleep Paralysis
This is a brief inability to move or speak while falling asleep or waking up, lasting seconds to minutes. It resembles cataplexy but occurs during the transition to or from sleep. Sleep paralysis may also involve vivid and sometimes frightening visual, auditory, or tactile hallucinations, usually when falling asleep or waking up.
Fragmented Nighttime Sleep and Insomnia
Despite excessive daytime sleepiness, individuals with narcolepsy often struggle with disrupted nighttime sleep. They may wake multiple times at night for 10–20 minutes, exacerbating daytime fatigue. Nighttime disturbances may include insomnia, vivid dreams, sleep apnea, acting out dreams, and periodic leg movements.
REM Sleep Behavior Disorder (RBD)
Typically, during REM sleep, the body’s muscles are paralyzed to prevent physical reactions to dreams. However, individuals with RBD lack this paralysis, leading to actions such as punching, kicking, shouting, or grabbing while asleep. These behaviors can disturb their sleep and that of others. RBD may occur independently or as a symptom of a neurological condition like narcolepsy.
See more: Identifying Sleep Apnea Symptoms: Are You at Risk?
Causes of Narcolepsy
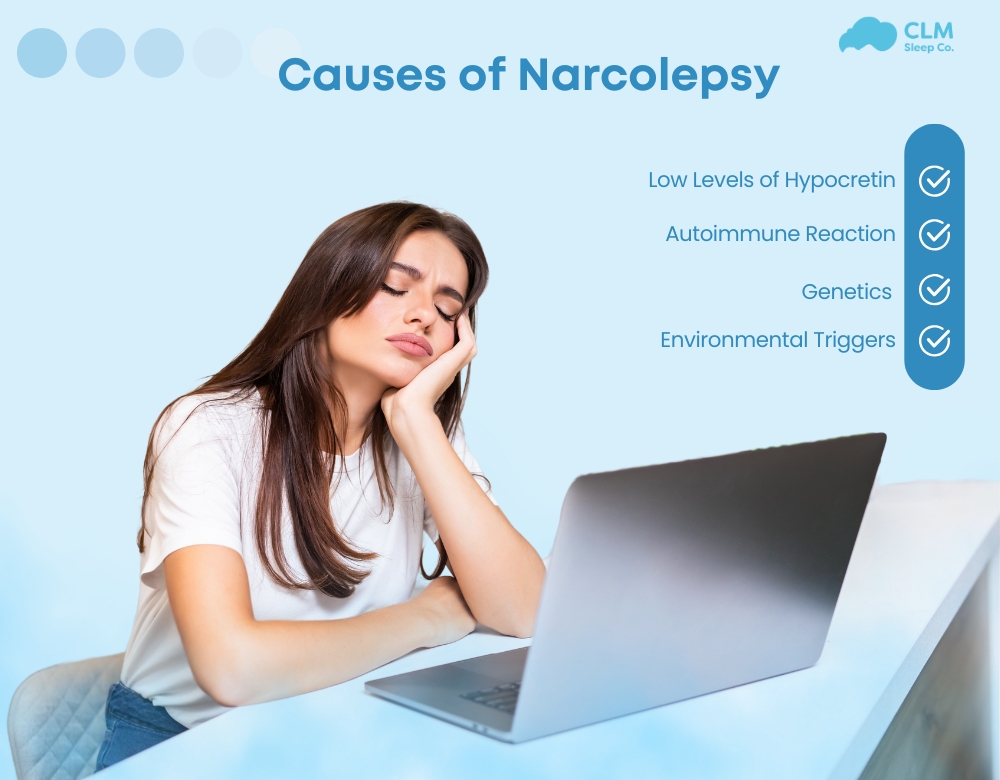
The exact cause of narcolepsy remains unknown. However, several factors are believed to contribute to the condition:
- Low Levels of Hypocretin (Orexin): People with Type 1 narcolepsy have significantly reduced levels of hypocretin, a brain chemical that regulates wakefulness and REM sleep. This reduction is commonly associated with cataplexy. The exact reason for the loss of hypocretin-producing cells is unclear. Still, it is suspected to result from an autoimmune reaction, where the immune system mistakenly attacks the body’s cells.
- Autoimmune Reaction: Experts believe that an autoimmune response may be responsible for destroying hypocretin-producing cells in the brain, leading to narcolepsy.
- Genetics: Genetics may also play a role in narcolepsy. However, the likelihood of a parent passing the condition to a child is very low, with only a 1% to 2% risk.
- Environmental Triggers: Narcolepsy has been linked to exposure to the H1N1 flu (swine flu) and, in some cases, to a specific type of H1N1 vaccine administered in Europe. These factors might trigger the condition in individuals predisposed to narcolepsy.
Diagnosis of Narcolepsy
The process of diagnosing narcolepsy involves a series of steps to ensure an accurate determination:
- Clinical Exam and Medical History: A doctor will conduct a thorough clinical examination and gather a detailed medical history. Patients may be asked to keep a sleep journal over one to two weeks, documenting sleep patterns and symptoms. This helps identify irregularities and assess the severity of symptoms.
- Physical Examination: A physical exam may be performed to rule out other neurological or medical conditions that could cause similar symptoms.
- Consultation with a Sleep Specialist: For a precise diagnosis, individuals are often referred to a sleep medicine specialist.
Specialized Tests for Narcolepsy
To confirm the diagnosis, two key tests are usually conducted in a sleep disorders clinic:
Polysomnogram (PSG or Sleep Study):
This overnight test monitors various physiological parameters during sleep, including brain activity, muscle movements, breathing, and eye movements. It helps determine if REM sleep occurs too early in the sleep cycle and checks for other conditions such as sleep apnea.
See more: Guide to Sleep Apnea Test At Home: Quick and Easy
Multiple Sleep Latency Test (MSLT):
Conducted during the day, this test measures how quickly an individual falls asleep and whether they enter REM sleep during several scheduled naps.
Additional Diagnostic Methods
- Hypocretin Level Testing:
In some cases, measuring the level of hypocretin-1 in the cerebrospinal fluid can aid in diagnosis. This requires a lumbar puncture (spinal tap) to collect a sample of cerebrospinal fluid for analysis. Low levels of hypocretin-1 are strongly associated with Type 1 narcolepsy.
See more: AHI index – Measures the severity of sleep apnea
Treatment Options for Narcolepsy
Although there is no cure for narcolepsy, its symptoms can be managed through a combination of medications and lifestyle adjustments. Treatment focuses on relieving symptoms rather than addressing the underlying condition. Each person’s treatment plan is unique, and it may take time to find the most effective combination.
People with narcolepsy are at a higher risk for heart disease and other heart-related issues, so regular monitoring of heart health is essential when considering medications or therapies.
Medications
Medications play a key role in managing symptoms. It may take time to identify the most effective drugs with the fewest side effects for each individual. Common treatments include:
- Wake-Promoting Agents:
Medications like modafinil, armodafinil, and solriamfetol are often the first choice for managing excessive daytime sleepiness (EDS). These central nervous system stimulants are less addictive and have fewer side effects compared to older stimulants, making them effective for improving alertness and reducing drowsiness. - Amphetamine-like Stimulants:
If wake-promoting agents are ineffective, doctors may prescribe stimulants like methylphenidate to reduce EDS. However, these drugs require careful monitoring due to potential side effects. - Antidepressants:
Tricyclic antidepressants (e.g., imipramine, desipramine, clomipramine, protriptyline) and selective serotonin and noradrenergic reuptake inhibitors (e.g., venlafaxine, fluoxetine, atomoxetine) are effective in managing cataplexy in many patients. - Sodium Oxybate:
Approved by the FDA for treating cataplexy and EDS, sodium oxybate (GHB) is tightly regulated due to safety concerns. A low-sodium version, mixed salt oxybate, includes calcium, magnesium, and potassium, offering a safer alternative for long-term use. - Histamine 3 Receptor Antagonist/Inverse Agonist:
Pitolisant, a non-scheduled medication available since 2019, is approved for treating EDS and cataplexy in adults and children over six. It increases histamine levels in the brain, helping manage symptoms.
Lifestyle Changes
In addition to medications, adopting certain lifestyle changes can significantly improve symptom management:
- Scheduled Naps:
Taking short, planned naps during the day helps reduce sleepiness. - Consistent Sleep Schedule:
Going to bed and waking up at the same time daily, including weekends, promotes better sleep. - Avoid Caffeine, Alcohol, and Smoking:
Avoid these substances, especially in the hours leading up to bedtime. - Cognitive Behavioral Therapy (CBT):
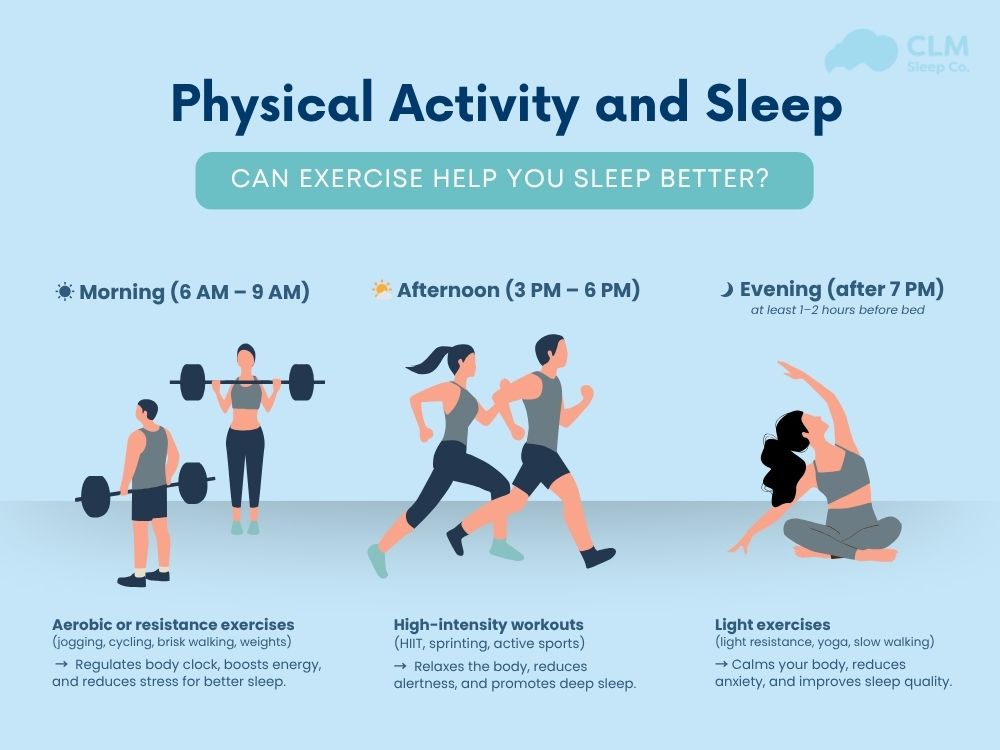
CBT can help improve sleep quality, reduce daytime sleepiness, and enhance overall health. - Exercise:
Regular physical activity, such as 20 minutes of exercise most days, at least 4–5 hours before bedtime, can improve sleep and reduce EDS. - Healthy Eating:
A heart-healthy diet is essential, especially given the increased risk of heart problems. Emerging research suggests a ketogenic diet (low carbs, high healthy fats) may help reduce EDS in Type 1 narcolepsy. Avoid heavy meals late in the day and refrain from eating close to bedtime. - Bedtime Relaxation:
Relaxing activities, such as warm baths, and maintaining a cool, comfortable sleep environment can promote restful sleep. - Safety Precautions:
Avoid driving when sleepy. Employers and schools are required under the ADA to accommodate individuals with narcolepsy by allowing flexible schedules or naps to manage symptoms effectively.
Support Groups
Support groups provide a space for individuals with narcolepsy and their families to connect, share experiences, and learn strategies for living with the condition.

How to Live with Narcolepsy
Living with narcolepsy can be challenging, but proper management strategies can improve daily life. Here are some tips for managing the condition:
- Educate family, friends, and coworkers: Help those around you understand the condition to foster support and empathy.
- Use assistive devices: Alarms, timers, and sleep-tracking apps can help maintain a consistent sleep schedule.
- Create a safe environment: To prevent injury during sudden sleep episodes, avoid dangerous activities like driving or operating heavy machinery without proper precautions.
- Seek emotional support: Joining support groups or talking to a mental health professional can provide coping strategies and reduce feelings of isolation.
See more: Effective Ways to Heal Sleep Apnea Naturally for Better Health
Conclusion of the article
Narcolepsy is a life-altering neurological disorder that affects sleep-wake cycles, leading to excessive daytime sleepiness and sudden sleep episodes. While there is no cure, proper treatment, lifestyle adjustments, and emotional support can significantly improve quality of life. Early diagnosis and treatment are essential to help individuals with narcolepsy maintain daily activities and personal well-being. If you or someone you know is experiencing symptoms of narcolepsy, seek guidance from a healthcare professional for proper diagnosis and management.
Living with narcolepsy doesn’t have to mean living without hope. By understanding the condition and accessing the right support, it’s possible to reclaim control over your daily life. If you or someone you know is experiencing symptoms of narcolepsy, don’t wait – explore your options today. Visit CLM Sleep for expert advice, treatment plans, and resources tailored to your needs. Let’s work together toward better sleep and brighter days! At CLM Sleep, we offer comprehensive diagnostic and treatment services for sleep apnea, helping you restore sleep quality and enhance your health. You can also explore other sleep improvement devices at Cpapdiscount.