Sleep apnea is a very common sleep disorder where a person stops breathing over and over again while they are asleep. If left untreated, it can contribute to various health problems. Continuous positive airway pressure (CPAP) therapy is one of the most effective treatments available. However, why is sleep apnea retesting necessary? Retesting on a periodic basis is essential to ensure that the treatment remains effective, especially as personal health conditions change. This post from CLM Sleep discusses the need for a retest in sleep apnea, key signs one needs to consider for a retest, and the types of sleep studies that are available, so one can manage it most effectively.
Why is sleep apnea retesting necessary?
Retesting is important as you have to continue to manage the condition as well as make sure that the current treatment is effective. The severity of sleep apnea can change due to changes in weight or lifestyle over time, aging, or having other new health conditions developed like diabetes or heart disease.
If left unchecked, untreated, or inadequately managed, sleep apnea can lead to serious complications, including high blood pressure, cardiovascular disease, daytime fatigue, and impaired cognitive function. Regular evaluations help healthcare providers determine whether adjustments to therapy – such as modifying CPAP settings, exploring alternative treatments, or addressing underlying causes – are needed to maintain optimal breathing during sleep.
Additionally, advancements in sleep medicine mean that new and improved treatment options may become available. A follow-up sleep study allows individuals to benefit from the latest therapies, improving both their sleep quality and overall health.
For these reasons, healthcare professionals often recommend periodic sleep apnea retesting to ensure long-term well-being and prevent potential health risks.
When should you consider sleep apnea retesting?
Several situations may warrant a retest for sleep apnea:
Changes in symptoms
If you notice a return or worsening of sleep apnea symptoms, this may indicate that your current treatment is no longer providing adequate relief. Symptoms to watch for include:
- Loud snoring that has become more frequent or intense
- Choking or gasping for air during sleep
- Excessive daytime fatigue, even after a full night’s rest
- Morning headaches, which can be a sign of poor oxygen levels during sleep
- Difficulty concentrating or memory issues, possibly due to disrupted sleep cycles
Sleep apnea retesting can help reassess the severity of your condition and determine if modifications to your treatment plan – such as CPAP pressure adjustments, alternative therapies, or lifestyle changes – are needed.
Worsening sleep apnea symptoms may signal ineffective treatment (Source: CLM Sleep)
Ineffective CPAP therapy
CPAP therapy is one of the most common treatments for sleep apnea, but its effectiveness can diminish over time. If you remain compliant with CPAP usage but still experience symptoms such as persistent fatigue, poor sleep quality, or morning headaches, a retest may be necessary.
- Factors that might necessitate a CPAP reassessment include:
- Changes in airway resistance, requiring modifications to pressure settings
- Mask discomfort or air leaks, reducing treatment effectiveness
- Nasal congestion or breathing difficulties interfering with CPAP delivery
A follow-up sleep study can determine whether CPAP adjustments, alternative devices (such as a BiPAP or APAP machine), or other treatments are necessary to restore optimal sleep quality.
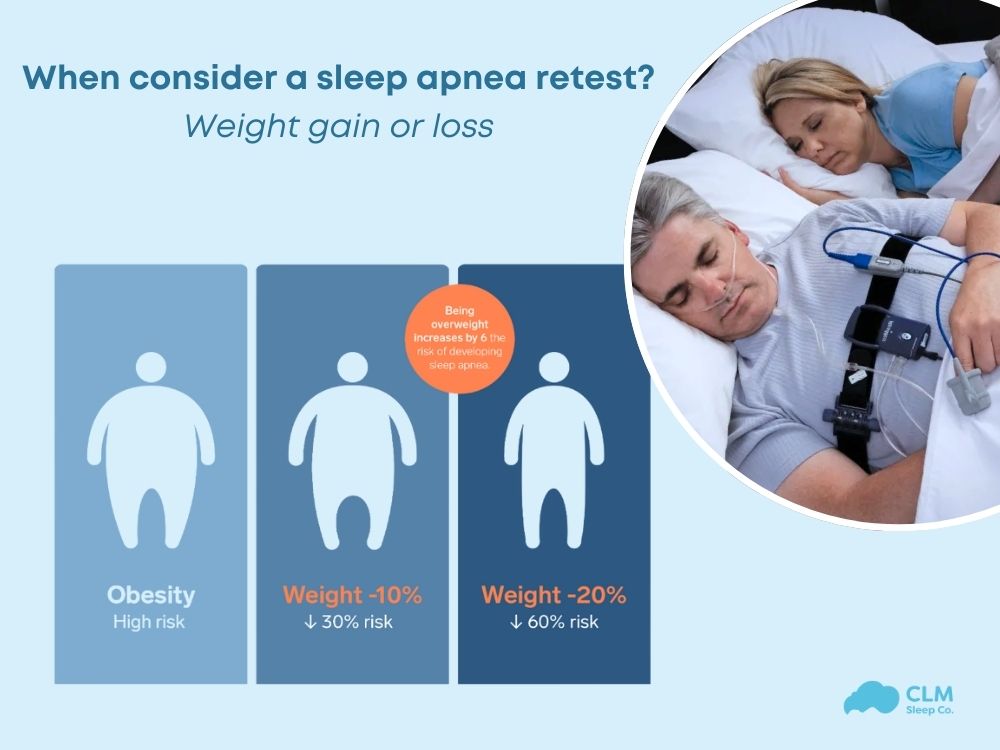
Weight gain or loss
Weight fluctuations can have a major impact on sleep apnea severity. The American Academy of Sleep Medicine recommends retesting if your weight has changed by 10% or more, as this can alter airway dynamics and affect treatment efficacy.
- Weight gain can lead to increased fat deposits around the upper airway, worsening airway obstruction and potentially necessitating higher CPAP pressure or alternative treatments.
- Weight loss may reduce sleep apnea severity, possibly eliminating the need for CPAP or allowing for lower pressure settings.
A retest can assess how these changes have influenced your condition and guide necessary treatment adjustments.
Post-surgery evaluation
If you have undergone surgery that affects the airway, a sleep apnea retest may be recommended to evaluate its impact. Surgical procedures that could influence sleep apnea include:
- Bariatric surgery (weight loss surgery), which may lead to a reduction in apnea severity
- Nasal surgeries (such as septoplasty or sinus surgery) to improve airflow and reduce nasal congestion
- Upper airway surgeries (such as tonsillectomy, UPPP, or Inspire therapy) designed to alleviate airway obstruction
A follow-up sleep study can help determine whether surgical interventions have improved or resolved sleep apnea and whether CPAP therapy or other treatments should be adjusted accordingly.
New health conditions
If you develop new health conditions, particularly those related to cardiovascular or metabolic health, a sleep apnea retest may be necessary. Conditions that may warrant a reevaluation include:
- High blood pressure (hypertension) that remains uncontrolled despite treatment
- Heart disease or irregular heart rhythms (arrhythmias), which can be worsened by untreated sleep apnea
- Type 2 diabetes or metabolic syndrome, which are linked to sleep apnea severity
- Chronic respiratory conditions, such as COPD or asthma, that may affect breathing during sleep
Because untreated sleep apnea can contribute to the progression of these conditions, a retest ensures that therapy remains effective in preventing further complications.
Routine monitoring
Even in the absence of new symptoms or health changes, periodic sleep apnea retesting is recommended as part of long-term care. Sleep apnea is a dynamic condition that can evolve, and regular evaluations help:
- Monitor progression or improvement of the disorder
- Ensure ongoing treatment effectiveness
- Identify potential new therapy options, including advances in CPAP technology or alternative treatments
Healthcare providers often recommend a follow-up sleep study every few years, particularly for individuals with moderate to severe sleep apnea, to ensure optimal management of the condition.
How Often Should You Have A Sleep Apnea Test?
According to research from the University of Rochester Medical Center, if no significant abnormalities are observed in the body when experiencing sleep apnea, you should repeat a sleep study every five years to ensure that treatments like CPAP remain effective and are appropriately set. This timeframe may vary depending on the severity of sleep apnea and any abnormalities in the body.
For individuals with mild to moderate sleep apnea, retesting every 1 to 3 years may be necessary to monitor the condition and adjust treatment if needed.
For those with severe sleep apnea, more frequent evaluations are required, approximately every 1 to 2 years. Severe sleep apnea has a significant impact on overall health, particularly increasing the risk of cardiovascular diseases, high blood pressure, and a very high likelihood of stroke.
However, if you experience significant weight fluctuations, newly developed conditions such as high blood pressure, or serious events like a heart attack or stroke, immediate retesting may be required to adjust the treatment plan accordingly.
See more: How to determine the severity of sleep apnea using the AHI sleep apnea index?
What are the common types of sleep studies?
To diagnose or reassess sleep apnea, healthcare providers may recommend one of the following sleep studies:
In-lab sleep study (Polysomnography)
Polysomnography (PSG) is a comprehensive sleep study conducted in a sleep laboratory. It provides detailed monitoring of various physiological parameters during sleep, including:
- Brain activity (EEG)
- Eye movement (EOG)
- Heart rate and rhythm (ECG)
- Muscle activity (EMG)
- Breathing patterns and oxygen level
This type of study is considered the gold standard for diagnosing sleep disorders, as it provides extensive data that can guide treatment decisions
Home sleep apnea test (HSAT)
A Home Sleep Apnea Test (HSAT) allows patients to undergo sleep monitoring in the comfort of their own homes. These tests typically focus on measuring breathing parameters, such as:
- Airflow
- Oxygen saturation
- Respiratory effort
- Snoring and body position
HSATs are more convenient and cost-effective than in-lab studies but may not capture as comprehensive a range of data. They are typically recommended for individuals with a high likelihood of moderate to severe obstructive sleep apnea.
Conclusion
Regular retesting for sleep apnea is essential to ensure that treatment remains effective, particularly as health conditions, lifestyle factors, and available therapeutic options change over time. Whether prompted by new symptoms, treatment inefficacy, weight fluctuations, or other factors, reassessing sleep apnea status helps optimize therapy and improve overall health. By staying vigilant and proactive, individuals with sleep apnea can enhance their quality of life, reduce health risks, and maintain restorative sleep for better well-being.
Source
University of Rochester Medical Center (URMC) 2021, ‘Sleep Studies at Jones Memorial’, URMC, <https://www.urmc.rochester.edu/MediaLibraries/URMCMedia/jones-memorial/services/images/783-You-Are-Having-A-Sleep-Study-2.pdf>.


