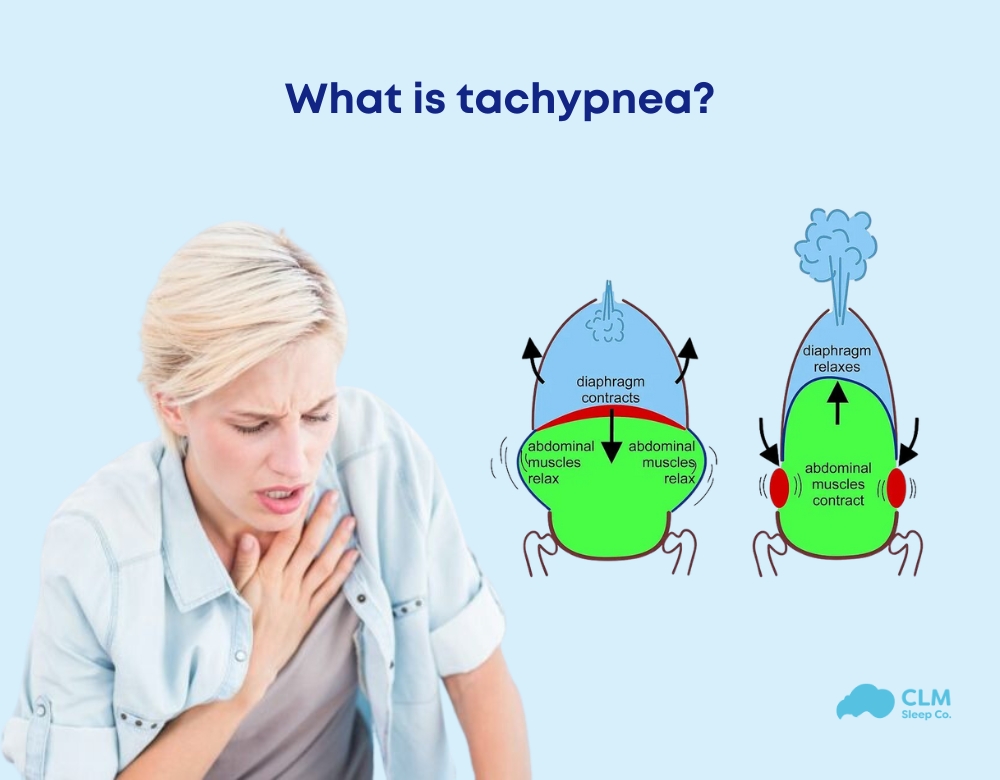
Tachypnea describes a rapid, shallow breathing pattern that may occur when the body has insufficient oxygen or excess carbon dioxide. It can be triggered by factors such as infections, asthma, overheating, and more. This breathing pattern can affect people of all ages, including newborns, children, and adults. While tachypnea is not a disease or condition, it can respond to both harmless situations, like physical activity, or underlying medical issues. This article from CLM Sleep explores the symptoms, causes, treatments, and other important details about tachypnea.
Overview about tachypnea
What is tachypnea? Tachypnea (pronounced “tuh-KIP-nee-uh”) is rapid, shallow breathing. When this fast breathing is temporary and resolves on its own, it is called transient tachypnea. Various medical conditions can lead to tachypnea.
This condition can affect people of all ages, including both infants and adults. It is especially common in preterm infants or adults with respiratory disorders such as asthma or COPD.
Rapid breathing is a natural response during physical activities such as exercise or intense efforts like running. However, tachypnea can also occur even when your body is at rest.
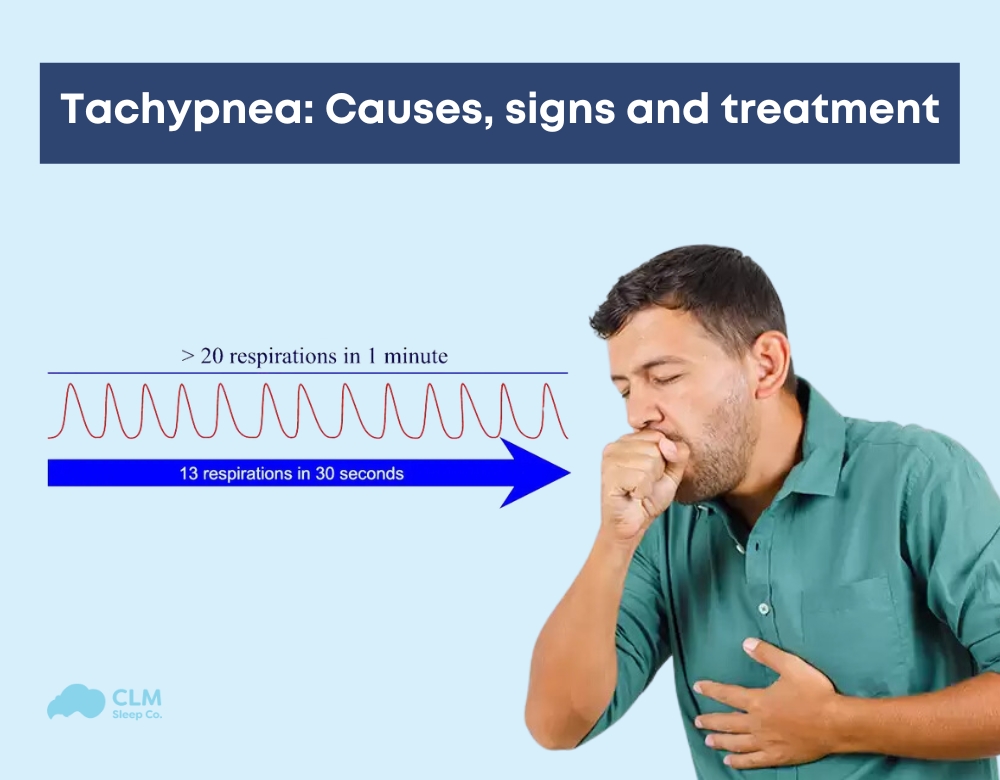
How do I know if I’m breathing too fast? You can measure your breathing rate at home by counting the number of breaths you take in one minute. For infants, a normal breathing rate ranges from 40 to 60 breaths per minute. For adults at rest, the normal range is 12 to 25 breaths per minute.
In newborns, transient tachypnea is indicated if their respiratory rate exceeds 60 breaths per minute. For adults, tachypnea may occur if you take more than 25 breaths per minute while at rest.
Symptoms
Tachypnea refers to rapid, shallow breathing. According to a 2021 study, the normal breathing rate for adults is 12–20 breaths per minute. Tachypnea is identified when the breathing rate exceeds 20 breaths per minute in adults.
In newborns, tachypnea is defined as a respiratory rate higher than 60 breaths per minute.
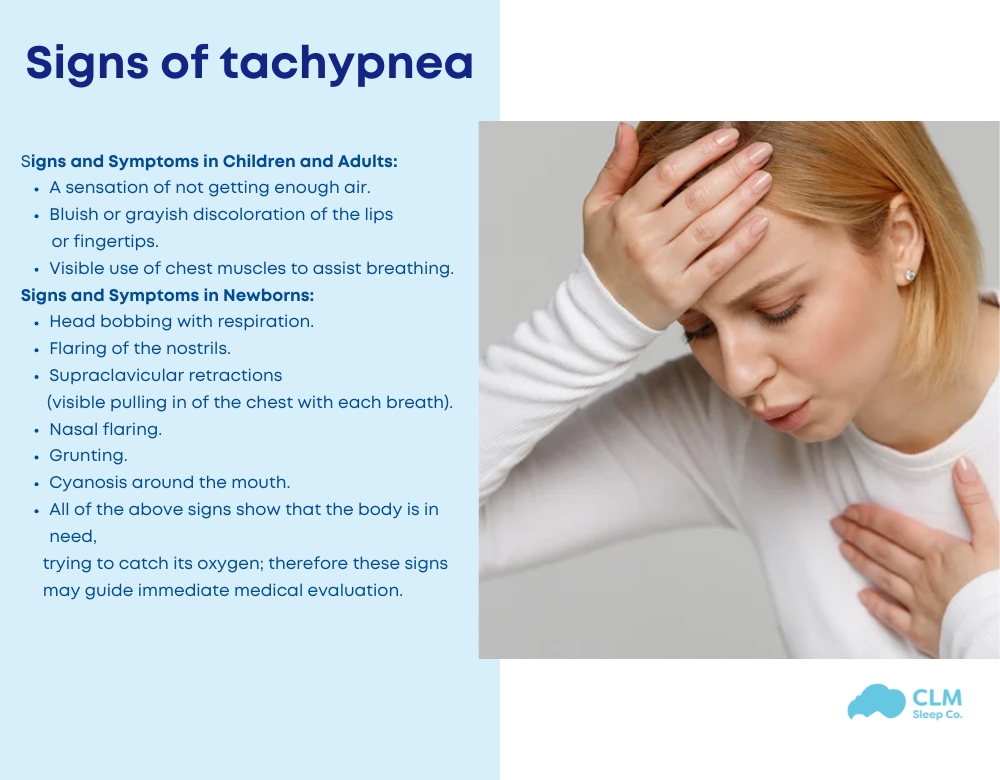
Signs and Symptoms in Children and Adults:
- A sensation of not getting enough air.
- Bluish or grayish discoloration of the lips or fingertips.
- Visible use of chest muscles to assist breathing.
Signs and Symptoms in Newborns:
- Head bobbing with respiration.
- Flaring of the nostrils.
- Supraclavicular retractions (visible pulling in of the chest with each breath).
- Nasal flaring.
- Grunting.
- Cyanosis around the mouth.
- All of the above signs show that the body is in need, trying to catch its oxygen; therefore these signs may guide immediate medical evaluation.
All of the above signs show that the body is in need, trying to catch its oxygen; therefore these signs may guide immediate medical evaluation.
Seek medical attention (see a doctor) if you have:
When to See a Doctor:
In Case of Severe or Worsening Symptoms:
- Respirations are fast and do not decrease with rest.
- Chest pain, dizziness, fainting confusion
- Blue skin, lips, or nails due to low levels of oxygen
Admixed Conditions:
- When the symptoms occur together with a high fever, severe coughing, or wheezing.
- In a person with preexisting conditions such as asthma, COPD, or heart problems wherein there is an increase in respiratory rate noticed.
For Infants and Children:
- Your baby or child breathes faster than normal while resting.
- Signs like grunting, flaring nostrils, or trouble feeding accompany rapid breathing.
Always consult a healthcare provider to address the cause of rapid breathing, especially if it persists or is associated with other concerning symptoms.
Causes
Tachypnea can occur as a symptom of various medical conditions, including:
- Allergic Reactions
- Anxiety or Panic Disorders
- Asthma
- Blood Clots
- Carbon Monoxide Poisoning
- Chronic Obstructive Pulmonary Disease (COPD)
- Diabetic Ketoacidosis
- Pleural Effusion (fluid buildup around the lungs)
- Pneumonia
- Pulmonary Embolism (a blood clot in the lungs)
- Sepsis
Causes of Tachypnea in Newborns
Before birth, a baby’s lungs are filled with fluid. Hormonal changes during labor help the lungs absorb this fluid, and most of it is expelled during a vaginal delivery. If this process occurs too slowly, the excess fluid remains in the lungs, leading to tachypnea. This condition is often temporary but requires careful monitoring.

Treatment
Treatment for tachypnea depends on its underlying cause. Because the condition itself is a symptom, a doctor will focus on identifying and addressing the root problem.
If the cause is not already known, the doctor may perform various tests, review the patient’s medical history, and assess accompanying symptoms.
Diagnostic Steps May Include:
- Listening to lung sounds using a stethoscope.
- Measuring oxygen levels with a pulse oximeter placed on the finger.
- Conducting blood tests to evaluate acid levels, glucose, blood counts, or electrolyte imbalances.
- Performing imaging tests, such as a chest CT scan, chest X-rays, or brain MRI.
- Screening for toxins or poisons.
- Conducting pulmonary function tests to assess lung performance.
Treatment Options Based on the Cause:
- Asthma or COPD: Inhaled medications, such as bronchodilators, to open the airways.
- Bacterial Pneumonia: Antibiotics to combat the infection.
- Viral Pneumonia: Antiviral medications, such as antibiotics, are ineffective against viruses.
- Other Causes: Treatments tailored to specific conditions, such as blood clot management, oxygen therapy, or metabolic stabilization.
The approach to treatment will vary based on the patient’s diagnosis, ensuring that the underlying issue is effectively managed.

The relationship between tachypnea and sleep apnea
Tachypnea and sleep apnea are distinct but related breathing conditions that can influence each other. Tachypnea refers to rapid, shallow breathing, often caused by conditions like respiratory issues, anxiety, or metabolic imbalances. Sleep apnea, on the other hand, involves repeated pauses or shallow breathing during sleep due to airway obstruction or brain signaling issues.
After an apnea episode, the body may compensate with a period of rapid breathing, resembling tachypnea. Both conditions can lead to oxygen imbalances, strain on the cardiovascular system, and overlapping symptoms, especially in individuals with underlying respiratory or metabolic disorders.
Conclusion of the article
Tachypnea is rapid shallow breathing that can result from a respiratory cause or a metabolic cause. While it may be only an initial response, persistent tachypnea calls for a full medical investigation to identify and treat the underlying cause. Specific diagnosis and specific treatment such as drugs or oxygen therapy are important in the management of this condition.
Patients experiencing sleep-related breathing disorders like those related to tachypnea or possible tachypnoea-sleep apnoea overlap should receive specialized care. CLM Sleep provides full sleep studies and treatments customized to help with irregular breathing and enhance overall respiratory health. Improved patient health outcomes are made possible by careful study of the relationship between sleep and respiration in such patients and related conditions.