Sleep apnea is a grave sleep disorder in which a person’s breathing repeatedly stops and starts during sleep, often resulting in fragmented rest and at times many associated health issues. But what causes sleep apnea? With CLM Sleep
What cause obstructive sleep apnea (OSA)
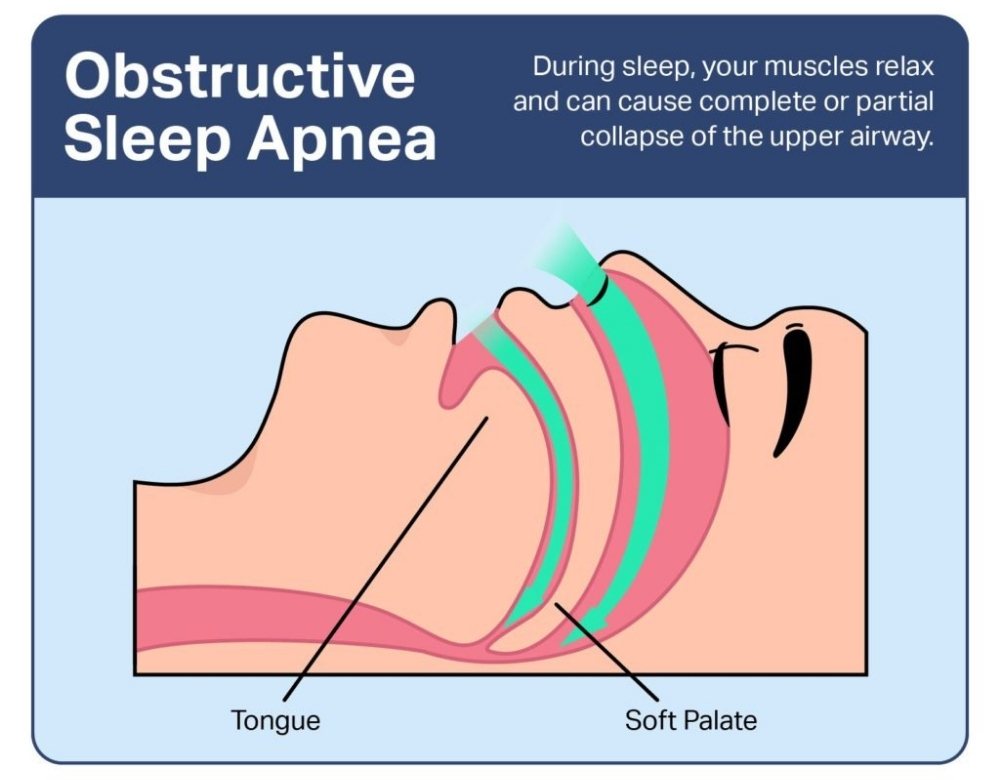
Obstructive Sleep Apnea (OSA)
Obstructive Sleep Apnea (OSA) is a common, and the most important types of sleep apnea your breathing stops during sleep because air cannot flow into the lungs through the mouth and nose for at least 10 seconds on at least 5 instances per hour with one or more of the following associated episodes: choking or gasping, or respiratory effort-related arousals.
See more: Identifying Sleep Apnea Symptoms: Are You at Risk?
Information about obstructive sleep apnea
The term “apnea” comes from a Greek word meaning “breathless”- in OSA, what happens is the muscles at the back of the throat relax too much leading to a temporary airway collapse. There are several subscales in response to eight items: snoring, breathlessness, headaches upon waking up, getting up at night to urinate, sleepiness during daytime activities or that the patient has fallen asleep during driving, eating meals or talking with others, fatigue, and body mass index. This lack of oxygen then triggers a survival reflex that causes people to wake up just enough to resume breathing for a few seconds. She or he has sometimes repeated episodes of upper airway closure during sleep measured by complete sensor obstruction or airflow cessations.
While a reflex like this will keep you alive it also keeps waking you up periodically, laboring your sleep. In the long run, untreated OSA can result in other related health problems such as heart disease, and hypertension plus added chances of stroke. Effective control and management for OSA comes with understanding its pathophysiologic changes and manifestations.
See more: Sleep Apnea Symptoms in Women
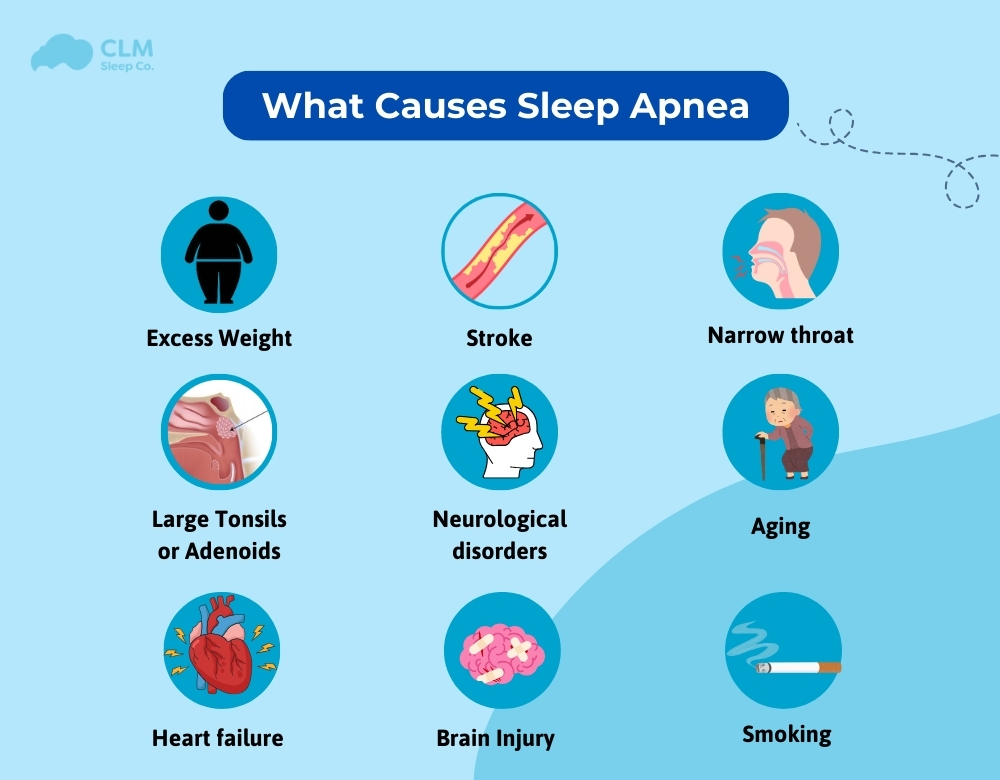
What causes obstructive sleep apnea?
This condition is a result of excessive relaxation of head and neck muscles, with surrounding soft tissues pressing against the windpipe. This leads to an obstruction to the airflow, with air finding no free passage into the lungs. This kind of obstruction results in repeated episodes of breath cessations, disrupted sleep, and several associated health problems. Typically, people with OSA make loud snoring sounds and have some kind of gasping or choking feeling while asleep, which has a serious impact on their overall health and quality of life.
See more: Sleep Apnea Is It Hereditary?
Central Sleep Apnea (CSA)
Central Sleep Apnea (CSA) is defined as a cessation of breathing during sleep for 10 seconds or longer caused by a lack of respiratory effort.
Information about obstructive sleep apnea
Unlike Obstructive Sleep Apnea (OSA), which is due to upper airway obstruction, in CSA, there is a transient failure of the brain’s respiratory rhythm center. It is far less common than OSA and is often centrally triggered by several disorders including heart failure, stroke, or other diseases of the central nervous system. Symptoms reflecting inadequate sleep quality are dyspnea, some disturbance of sleep, and excessive daytime hypofunction. Some drugs may also induce them or even sleep at a high altitude. The management of CSA would involve identifying and correcting any underlying health issues. This helps to control breathing throughout sleep; one may be advised to use the CPAP or ASV.
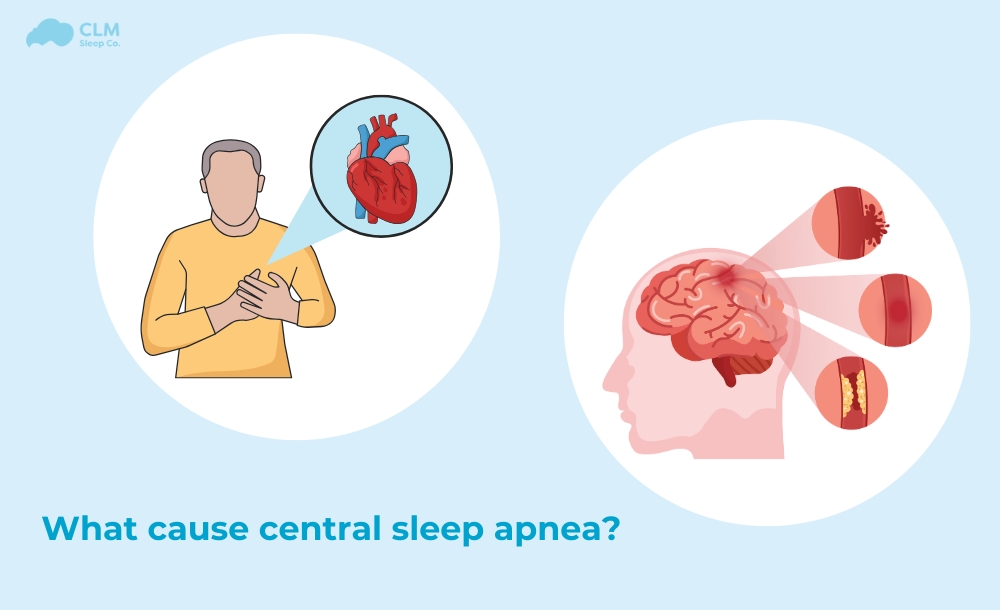
What can cause central sleep apnea?
Some potential causes of central sleep apnea may include:
- Heart Failure: When the heart can’t pump blood effectively, it disrupts normal breathing patterns.
- Low Blood Oxygen Levels (Hypoxia): Conditions such as high altitude can reduce oxygen levels and cause CSA.
- Nervous System Damage: Damage to parts of the brainstem or spinal cord that are critical for controlling breathing can cause CSA.
- Treatment for Obstructive Sleep Apnea: In some cases, using continuous positive airway pressure (CPAP) to treat obstructive sleep apnea can inadvertently cause central sleep apnea, although this condition can usually be resolved with continued CPAP use.
- Nervous System Conditions: Conditions such as amyotrophic lateral sclerosis (ALS) affect the brain’s ability to regulate breathing effectively.
People with central sleep apnea may not have the classic symptoms of obstructive sleep apnea, such as snoring, but they may experience pauses in breathing during sleep, leading to disrupted sleep and daytime sleepiness.
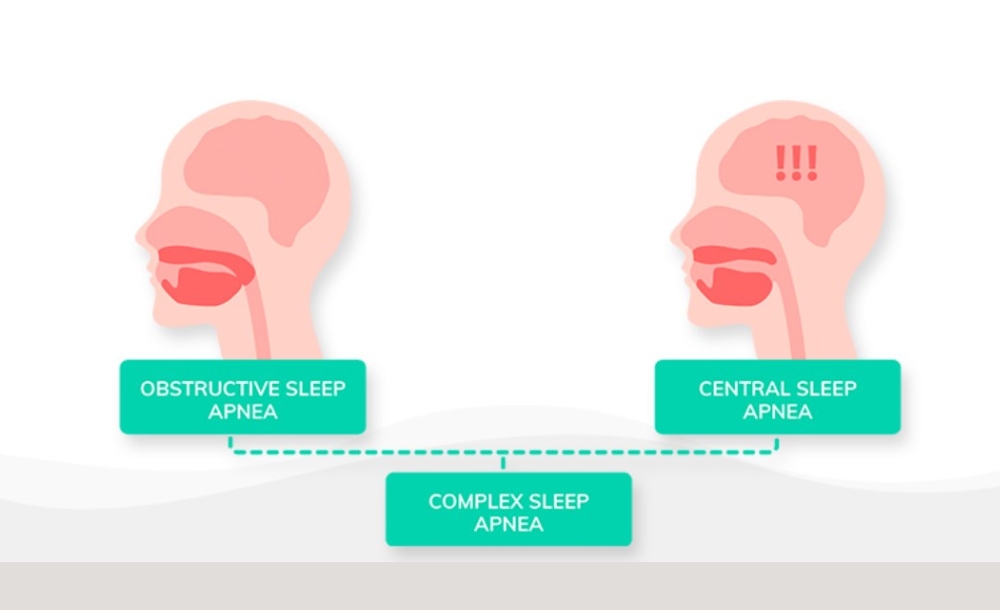
What cause Complex Sleep Apnea?
This mixed nature of apnea is characterized by both obstructive sleep apnea (OSA) and central sleep apnea (CSA). In these patients, episodes of obstructive sleep apnea are followed by those of central sleep apnea. This observation suggests that even when the obstruction is managed by a CPAP machine and the airway is clear, the brain may not signal appropriately to maintain normal breathing, thus leading to an episode of CSA.
Complex sleep apnea is discovered when patients with OSA continue to display symptoms even after the obstruction has been removed. This condition is rather more difficult to manage, as it calls for the management of issues about both the physical airway obstruction and the problems with neural signaling. Continuous positive air pressure turns out to be one of the aspects aided for symptom management of complex apnea. Other considerations include modifying the auto-titrating CPAP settings and appropriate management of other medical conditions.
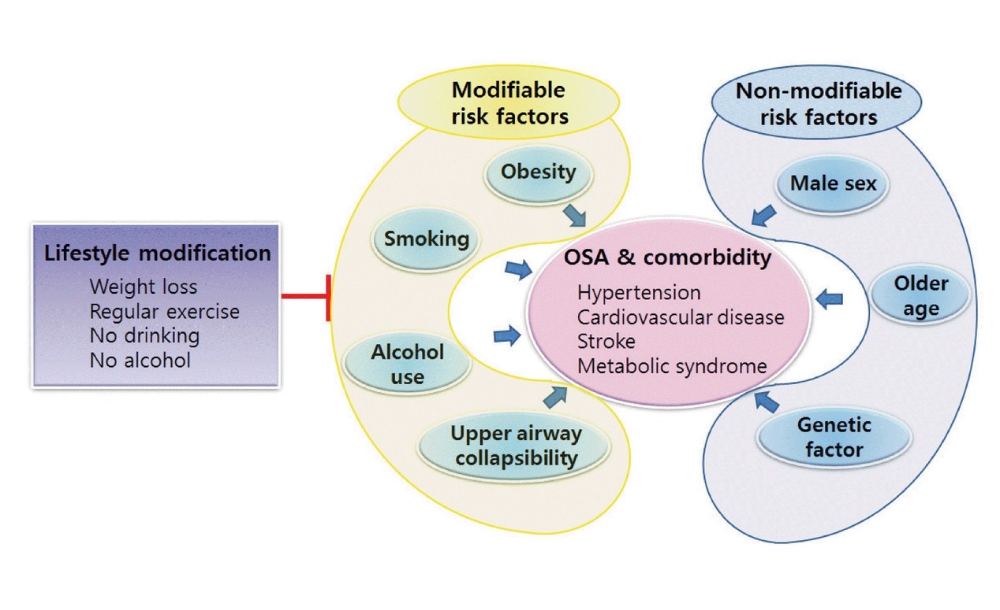
Contributing Factors
Several contributing factors can increase the risk of developing sleep apnea, particularly Obstructive Sleep Apnea (OSA). These include:
- Genetics: A family history of sleep apnea may increase the likelihood of developing the condition, as certain anatomical traits like narrow airways or enlarged tonsils can be inherited.
- Hormonal Disorders: Conditions like hypothyroidism or polycystic ovary syndrome (PCOS) can lead to changes in body structure or weight gain, increasing the risk of airway obstruction during sleep.
- Nasal Congestion: Chronic nasal congestion or structural issues, such as a deviated septum, can contribute to airway blockage, making it more difficult to breathe through the nose and worsening the symptoms of sleep apnea.

Lifestyle and Environmental Factors
Lifestyle and environmental factors can significantly influence the severity of sleep apnea symptoms. Key factors include:
- Sleep Position: Sleeping on the back (supine position) can cause the tongue and soft tissues to collapse backward, blocking the airway and worsening sleep apnea symptoms. Side sleeping is often recommended to alleviate this issue.
- Use of Sedatives or Muscle Relaxants: Medications like sedatives, tranquilizers, or muscle relaxants can relax the muscles of the throat, increasing the likelihood of airway obstruction during sleep.
- Smoking: Smoking irritates the upper airway, causing inflammation and fluid retention, which can narrow the air passages. Smokers are more prone to developing sleep apnea, and quitting smoking can reduce symptoms.
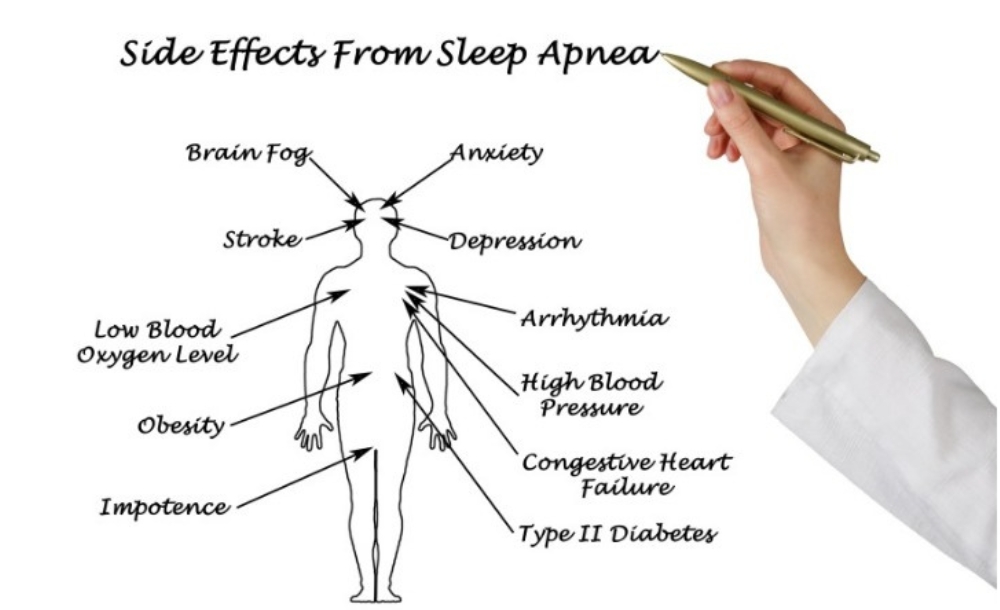
Impact of Sleep Apnea
Sleep apnea can have a range of serious consequences that impact both physical and mental health. Here are some key consequences associated with the condition
Daytime Symptoms
- Excessive Daytime Sleepiness: Many individuals with sleep apnea experience severe daytime fatigue due to disrupted sleep, leading to decreased productivity and increased risk of accidents.
- Difficulty Concentrating: Cognitive impairments, including trouble focusing and poor memory, are common in those suffering from sleep apnea.
- Memory Loss: Disrupted sleep can negatively affect memory consolidation and lead to memory lapses.
Mood and Mental Health
- Depression: The chronic fatigue and stress associated with sleep apnea can contribute to mood disorders, including depression.
- Irritability or Frustration: Mood swings and irritability can occur due to lack of restorative sleep and the impact of chronic fatigue.
Physical Symptoms
- Pauses in Breathing: Sleep apnea is characterized by repeated interruptions in breathing during sleep, which can last for several seconds to minutes.
- Snoring: Loud snoring is a common symptom of sleep apnea and can disrupt both the sufferer’s and their partner’s sleep.
- Morning Headaches: Frequent morning headaches can occur due to changes in carbon dioxide levels in the blood from interrupted breathing.
- Dry Mouth Upon Awakening: People with sleep apnea often breathe through their mouths during the night, leading to dryness upon waking.
Health Risks
- Heart Disease: Sleep apnea is linked to an increased risk of cardiovascular problems, including heart disease and heart failure.
- High Blood Pressure: The stress on the body caused by sleep apnea can lead to hypertension, which may require medical management.
- Stroke: The increased risk of cardiovascular issues from sleep apnea can lead to a higher likelihood of experiencing a stroke.
- Type 2 Diabetes: Sleep apnea is associated with insulin resistance, which can increase the risk of developing type 2 diabetes.
- Sexual Dysfunction: Sleep apnea can contribute to sexual issues, including reduced libido and erectile dysfunction in men.
Sleep-Related Issues
- Obstructive Sleep Apnea and Hypertension: Obstructive sleep apnea specifically has been shown to cause hypertension due to the stress placed on the cardiovascular system during episodes of apnea.
- Insomnia: Many individuals with sleep apnea also struggle with insomnia due to fragmented sleep patterns.
Other Effects
Weight Gain: Hormonal imbalances caused by sleep apnea can lead to weight gain and make it harder to lose weight.
See more: Can Sleep Apnea Cause Weight Gain?
Diagnosis and Treatment
Sleep apnea is a serious condition that can have a significant impact on a person’s quality of life if left untreated. Diagnosing sleep apnea often involves a combination of medical history, physical examination, and sleep studies. Once diagnosed, there are various treatment options available depending on the severity and cause of the condition. These can range from lifestyle changes to medical devices and even surgery.
Diagnosing sleep apnea
Diagnosing sleep apnea typically involves the following steps:
Medical History and Physical Examination: Your healthcare provider will review your symptoms, sleep patterns, and medical history. They may check for risk factors like obesity, high blood pressure, or a family history of sleep apnea.
Sleep Studies (Polysomnography):
- In-Lab Polysomnography: This is the most comprehensive method to diagnose sleep apnea. It involves an overnight stay in a sleep lab where your breathing, heart rate, oxygen levels, and brain activity are monitored while you sleep.
- Home Sleep Apnea Testing: A simplified version of polysomnography that can be done at home. It measures airflow, breathing patterns, and oxygen levels, though it may not be as detailed as an in-lab test.
Oxygen Level Testing: Some devices measure blood oxygen levels during sleep to detect drops in oxygen, a sign of sleep apnea.
Treatment of Sleep Apnea
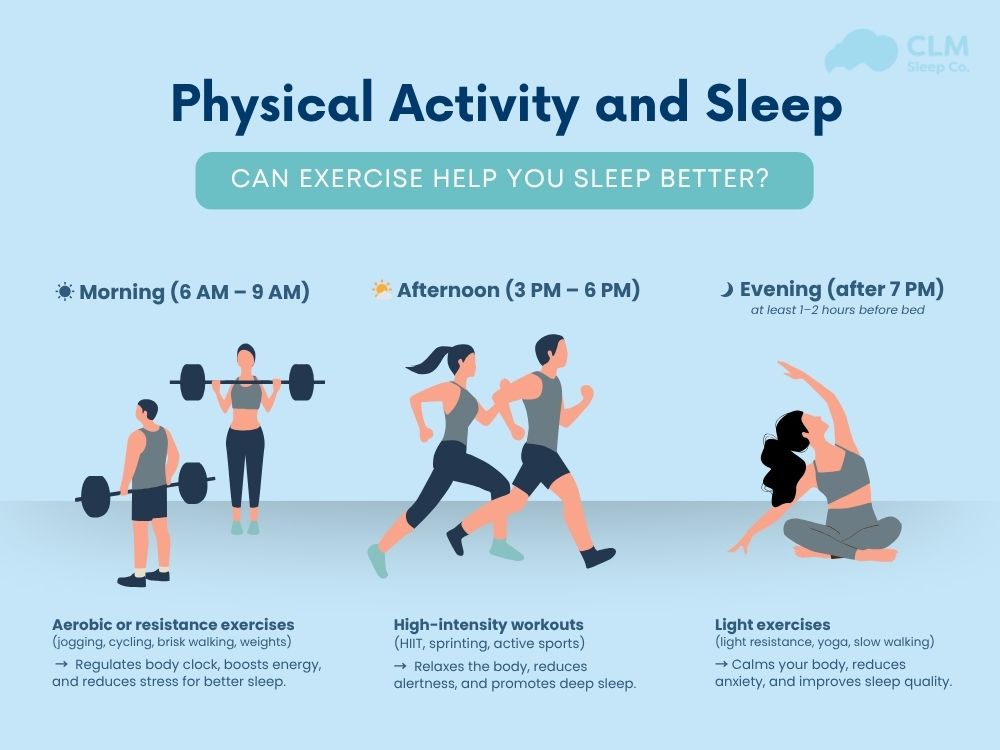
Lifestyle Modifications:
- Weight Loss: Here is the famous For individuals with obstructive sleep apnea (OSA), losing weight can reduce the pressure on the airway.
- Change in Sleep Position: Sleeping on your back can worsen OSA; side-sleeping can alleviate it.
- Avoiding Alcohol and Sedatives: These substances relax the muscles in the throat, worsening apnea.
See more: Effective Ways to Heal Sleep Apnea Naturally for Better Health
Continuous Positive Airway Pressure (CPAP):
- CPAP Therapy: This is an OSA treatment. A CPAP machine delivers constant air pressure through a mask to keep your airway open during sleep.
- BiPAP: Similar to CPAP but offers two levels of air pressure – higher when you inhale and lower when you exhale. This may be used for central sleep apnea (CSA).
Oral Appliances:
Mandibular Advancement Devices (MADs): Dental devices that push the lower jaw forward to keep the airway open. They are useful for mild to moderate cases of OSA.
Surgery:
- Uvulopalatopharyngoplasty (UPPP): Removes excess tissue from the throat to open the airway.
- Genioglossus Advancement: Repositions the tongue muscle attachment to prevent airway collapse.
- Maxillomandibular Advancement: Moves the jaw forward to enlarge the space behind the tongue and soft palate.
Implantable Devices:
Hypoglossal Nerve Stimulation: A surgically implanted device stimulates the nerve that controls tongue movement, keeping the airway open during sleep.
Treatment for Central Sleep Apnea:
- Adaptive Servo-Ventilation (ASV): This device adjusts the pressure based on your breathing patterns to treat CSA.
- Treating Underlying Conditions: For CSA caused by heart failure or nervous system damage, addressing the root condition is critical.
- Supplemental Oxygen: Some individuals with CSA may benefit from oxygen therapy to maintain proper oxygen levels during sleep.

See more: What Are Some Sleep Apnea Help Without CPAP?
Conclusion of the article
In this article, we have told you what causes sleep apnea. At CLM Sleep, we offer comprehensive diagnostic and treatment services for sleep apnea. Our goal is to help you restore sleep quality and enhance your health. You can also explore other sleep improvement devices at Cpapdiscount.